In previous newsletters, we’ve addressed the issue of physician burnout crisis in the US, with a doctor burnout rate of over 50%, as reported in the Medscape Physician Burnout and Depression Report 2023. The medical specialties with the highest burnout rates are Emergency Medicine, Internal Medicine and Pediatrics. Healthcare organizations, leadership roles, and support significantly contribute to physician burnout by imposing excessive workloads, inefficient work processes, and clerical burdens.
Yet physicians have minimal training in management and little on-the-job training skills to develop management skills such as how to allocate short and long term resources.

Management also relates to funding, advocacy and allocation of resources. With respect to funding for POCUS programs, we share several pearls from our webinar in July on funding and how to obtain funding.
Exploring potential sources for POCUS funding within your organization
-
CME dollars
-
Internal funding:
-
Internal grant funding (POCUS is innovation and improves quality of care metrics)
-
Research dollars
-
-
External funding:
-
Philanthropy
-
External grant funding
-
-
Existing resources: “Turning over the rocks”
-
SIM Center
-
Leverage industry – Vendors
-
Preparing a pitch – How to make the ask?
1) Creating a Reasonable Budget
-
Probes + Training is minimum
-
Look ahead: 3-5 yrs
2) Know Your Audience:
-
ACGME Guidelines (Required in EM, and now FM)
-
POCUS is happening! Don’t get left behind!
-
Safety! Risk reduction, Security Risk
-
Research? Get your baseline prior to submission
-
Improve retention
3) Organizational Direction – aligning the benefits of POCUS with values of the organization
-
Improving Quality of Care – “What you do serves as the proof of what you believe!” – Simon Sinek
-
Earlier Diagnosis, decreases unnecessary visits
-
Comparability across health centers
-
Residency driven, Faculty development
-
Search your 990’s (Guidestar, Propublica for free)
 Case Study #1
Case Study #1
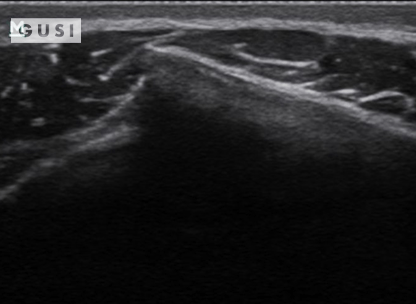
A 25-year-old male Taekwondo competitor from Africa experienced significant pain and tenderness in his right flank after receiving a forceful kick during the 2017 World Taekwondo Championships held in Muju, Korea. An immediate POCUS at the venue indicated a fracture in his 8th rib on the right anterior side of his chest.
A B
 |
 |
|
C 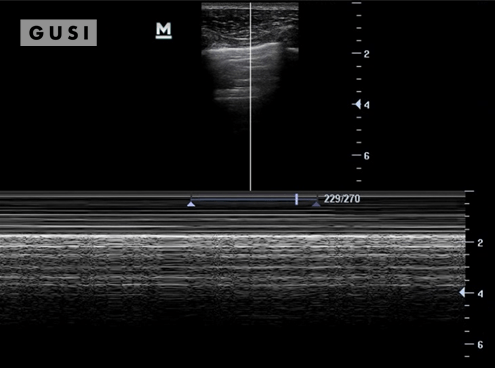 |
 |
A: The rib showed angular displacement in the longitudinal view.
B: In the transverse view, the rib appeared displaced.
C: Subsequent chest ultrasound scans did not detect a pneumothorax, and the athlete had no breathing difficulties with stable vital signs.
Initial on-site management was conservative, and the athlete later sought additional treatment from his sports doctor back home. His team’s physiotherapist confirmed the fracture through an x-ray during a subsequent check-up. He fully recovered in a few weeks without facing any setbacks.
 Case Study #2
Case Study #2
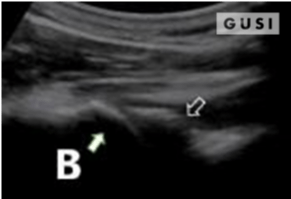
During the 2018 World Taekwondo Junior Championships in Hammamet, Tunisia, a 17-year-old male junior Taekwondo athlete took a fall, landing on his right shoulder. He exhibited a markedly limited range of motion in the affected shoulder and experienced intense pain, leading to suspicions of a dislocation.
 |
 |
|
 |
 |
A pre-reduction ultrasound (A) of the right shoulder showed a pronounced gap between the humeral head (indicated by a solid arrow) and the glenoid (marked by an open arrow), suggesting an anterior dislocation. Following a shoulder reduction procedure, a post-reduction ultrasound (B) verified the successful realignment of the glenohumeral joint (solid arrow pointing to the humeral head and open arrow to the glenoid).
After the procedure, the athlete displayed a considerably improved range of motion in his right shoulder and his pain levels diminished significantly.
 Case Study #3
Case Study #3
 |
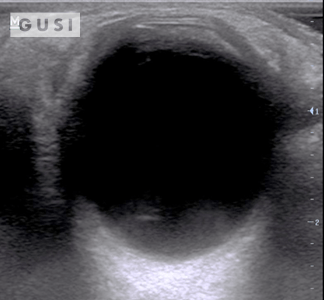 |
During the 2017 World Taekwondo Championships in Muju, Korea, a 30-year-old female athlete from Hong Kong was kicked in her left eye by an opponent. She reported fluctuating vision accompanied by pain during eye movement. A POCUS examination of the affected eye indicated a vitreous hemorrhage, with no evidence of lens subluxation or globe rupture.
On the ultrasound, as the athlete moved her eyes laterally, the hemorrhage (denoted by a white arrow) exhibited a swirling pattern within the globe, consistent with her eye movement. The athlete was promptly referred to a specialized medical center for an ophthalmology consultation, where the diagnosis of vitreous hemorrhage was confirmed. The patient was subsequently discharged from the Emergency Department with specific precautionary measures.
——-
To contribute valuable learning cases and propose future POCUS topics for our newsletters, please email [email protected] with the subject line “Newsletter.”
Dr. Jeong is the chairperson of the World Taekwondo (WT) Medical and Anti-doping Committee. He notably introduced point-of-care ultrasound to both World Taekwondo and the International Olympic Committee for the first time. His expertise encompasses the application of point-of-care ultrasound in primary care, sports medicine, and emergency & critical care medicine. He is credited with penning four book chapters on POCUS and has pioneered a curriculum in the area for various medical professionals, including international Taekwondo team doctors, attending physicians, sports medicine and pulmonology fellows, family medicine resident physicians, medical students, and APPs (PAs/NPs). Dr. Jeong’s acclaim in the field has led to invitations as a speaker, faculty member, and instructor at several international, national, and regional ultrasound conferences. Notably, he presented at the 2018 WONCA (World Organization of Family Doctors) World Conference in Seoul, Korea, and the 2019 World Congress on Ultrasound in Medical Education (WCUME) in Irvine, CA.
“As a family medicine and sports medicine physician, I can’t imagine covering sporting events without POCUS. POCUS is both a joy and a blessing to me. I always bring my handheld ultrasound to international sporting events. My athletes and coaches appreciate it when I show them their injuries on the ultrasound; it enhances their trust in me.”
GUSI in the Community
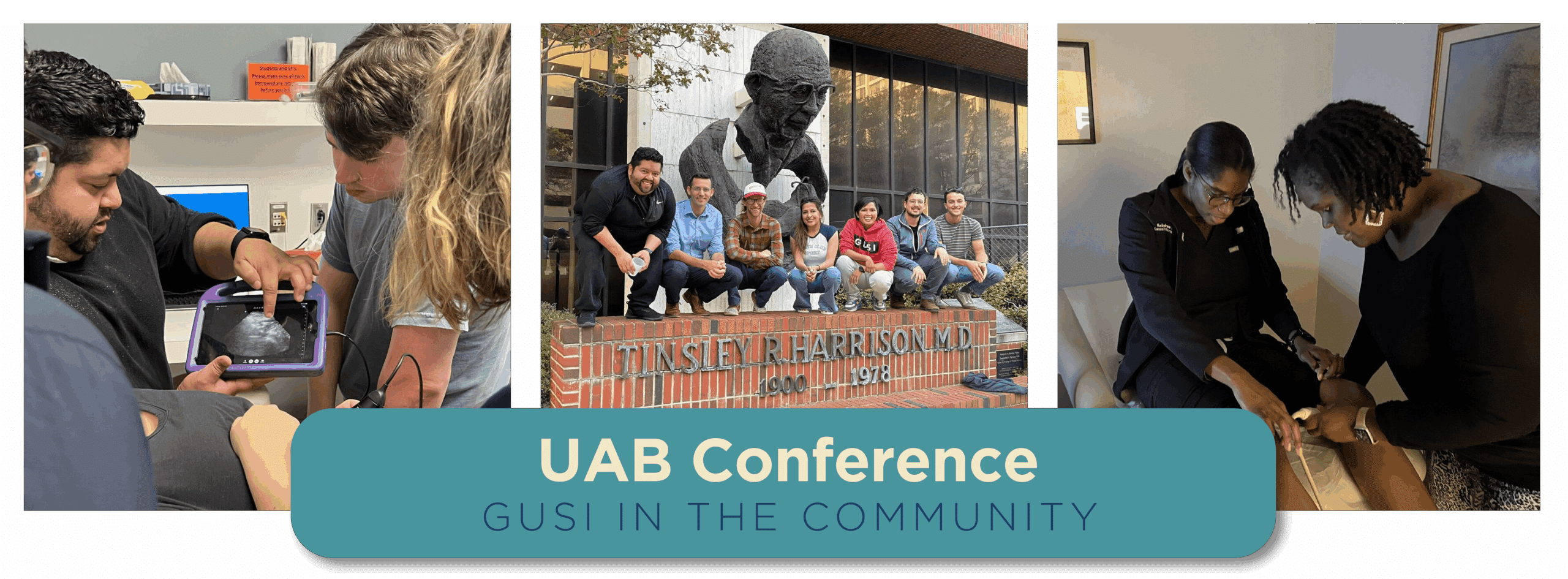
The GUSI Team successfully conducted a two-day, hands-on POCUS training session for a multidisciplinary group of doctors from the University of Alabama at Birmingham.

GUSI participated in the AAFP Family Medicine Experience, a premier event for family medicine. Our booth at FMX left attendees excited about the transformative potential of POCUS in bedside medicine.

Thanks to the World Congress on Ultrasound in Medical Education, we had the opportunity to introduce a significant initiative for training more than 500 midwives from 8 regions in basic Obstetric POCUS in Kenya. This project was made possible through a partnership with Butterfly Network, Inc., Kenyatta University, and the Bill and Melinda Gates Foundation. The oral presentation won 1st prize at the World Congress of Ultrasound in Medical Education Conference!

The Family Medicine Education Consortium collaborated with GUSI to provide practical training in POCUS fundamentals and various specific techniques to approximately 60 attendees at the FMEC 2023 Annual Meeting.
GUSI was thrilled to take part in the inaugural California Academy of Family Physicians POP event in Los Angeles. Our POCUS Workshop received positive feedback.
“People don’t buy what you do, they buy why you do it!”
–Simon Sinek–