Bridging the Maternal Care Gap with POCUS
In many rural areas of the Philippines, expectant mothers often face long travel times, high costs, and limited access to diagnostic tools. POCUS for Maternal Health in the Rural Philippines is changing that story. With handheld ultrasound devices and targeted training for local health workers, life-saving prenatal scans are now within reach for communities that need them most.
This article explores 10 powerful ways point-of-care ultrasound (POCUS) is bridging gaps in maternal health across the archipelago — and why it’s a game changer for women, babies, and healthcare providers alike.
Introduction
Point-of-care ultrasound (POCUS) is redefining maternal healthcare in underserved regions worldwide. In the Philippines, where rural communities face persistent challenges in accessing quality prenatal care, POCUS is becoming a game changer. This blog explores 10 powerful ways POCUS for maternal health in rural Philippines is closing diagnostic gaps, saving lives, and empowering frontline healthcare workers.
1. Bringing Ultrasound to Remote Villages
In many rural provinces of the Philippines, pregnant women may live several hours away from the nearest hospital with ultrasound services. This often means traveling by boat, motorbike, or jeepney across difficult terrain — a trip that can be both costly and physically exhausting for expectant mothers. The result? Many women simply skip essential scans altogether.
With POCUS for maternal health in rural Philippines, healthcare providers can now carry handheld devices directly into these communities. These lightweight, portable scanners can be connected to a tablet or smartphone, allowing midwives and rural doctors to perform pregnancy ultrasounds right inside barangay health stations or community clinics. This eliminates the need for long-distance travel, cuts costs for families, and ensures timely prenatal monitoring.
2. Detecting High-Risk Pregnancies Early
Conditions like placenta previa, breech presentation, multiple gestations, or abnormal placental attachment are leading contributors to maternal and neonatal complications. According to World Health Organization (WHO), many of these issues can be detected as early as the second trimester with a single quality ultrasound scan.
POCUS for maternal health in rural Philippines enables midwives, nurses, and general practitioners to identify these risks well before delivery. In one Philippine pilot project, over 31% of pregnant women scanned had an unsuspected complication that could have endangered them or their babies during birth. By catching these conditions early, rural healthcare workers can refer mothers to hospitals with surgical capacity, arrange safe transportation, and prepare necessary interventions before emergencies occur.
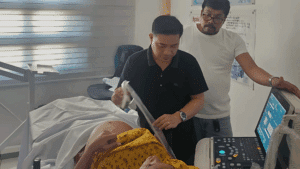
3. Empowering Community Health Workers
In the absence of OB-GYNs, rural midwives and nurses are often the primary — and sometimes only — healthcare providers for pregnant women in the Philippines. Unfortunately, their traditional toolkit is limited to blood pressure cuffs, fetal dopplers, and physical assessments, which cannot reveal many dangerous conditions.
Through targeted training programs like the Catanduanes Ultrasound Fellowship, these frontline providers are now learning how to perform and interpret obstetric POCUS. Even with short, focused training, studies show midwives can achieve diagnostic agreement rates of over 90% with experienced sonographers. This skillset gives them the confidence to make informed, immediate decisions and strengthens their role as trusted maternal health advocates within their communities.
4. Increasing Antenatal Visit Attendance
One of the most underestimated benefits of introducing POCUS into rural clinics is its impact on antenatal visit attendance. Expectant mothers are far more likely to attend regular checkups when they know they will see their baby’s image or hear the heartbeat — making each visit more engaging and meaningful.
Research from similar programs in Asia and Africa has shown a clear rise in prenatal visit compliance after POCUS was introduced. In the Philippines, local midwives report that expectant mothers often bring family members to witness the scan, creating a positive community culture around maternal health. The emotional connection and reassurance provided by ultrasound can transform antenatal care from a purely medical task into a bonding experience for both mother and family.
5. Improving Emergency Preparedness
Pregnancy complications often strike without warning, but many can be anticipated with proper screening. POCUS for maternal health in rural Philippines allows providers to detect risks — such as abnormal fetal positioning, signs of preterm labor, or low amniotic fluid — months before delivery.
By identifying these red flags early, rural clinics can prepare an emergency plan, secure transport to referral hospitals, and alert higher-level facilities in advance. In provinces where one doctor may serve tens of thousands of people, this proactive approach is lifesaving. It also prevents last-minute emergencies that place both mothers and healthcare systems under extreme pressure.
6. Reducing Maternal and Neonatal Mortality
Maternal mortality remains a serious challenge in the Philippines, with United Nations Children’s Fund (UNICEF) reporting that around 13 women die every day from pregnancy-related complications. Many of these deaths are preventable with timely diagnosis and intervention.
In rural pilot programs, handheld POCUS devices have been credited with reducing preventable maternal deaths by as much as 6% and neonatal deaths by nearly 15% through early detection of complications. When paired with timely referrals, these scans ensure high-risk pregnancies are managed in safer settings, leading to healthier outcomes for both mother and child.

7. Cost-Effective Technology for Low-Resource Settings
Traditional ultrasound machines can cost tens of thousands of dollars and require specialized facilities. In contrast, portable POCUS devices like the Butterfly iQ are far more affordable, require minimal infrastructure, and can be operated with a mobile phone.
For rural health units with tight budgets, this technology represents a game-changing investment. One device can serve hundreds of pregnancies per year, allowing continuous monitoring without the overhead of a full hospital-based imaging department. The low maintenance requirements also make them practical for clinics in remote or typhoon-prone areas, where resources are scarce and resilience is essential.
8. Real-Time Specialist Support with ScanHub
Even with basic training, some cases require specialist input. ScanHub enables rural providers to share scans instantly with remote experts for second opinions. This is especially valuable in the Philippines’ island provinces, where specialist access can be limited by geography.
Through secure cloud sharing, obstetricians and radiologists in urban centers can review images and provide feedback within minutes. This ensures accurate diagnoses, informed treatment plans, and continuity of care — all without requiring the patient to travel long distances for a consultation.
9. Simplified Scanning with ScanHub
ScanHub is GUSI’s mobile application (available on both the Apple App Store and Google Play Store) that enables even minimally trained providers to perform quality scans. Its intuitive design ensures POCUS for maternal health in rural Philippines can be integrated quickly into local clinics.
While traditional ultrasound training can take years, tools like ScanOne and ScanHub are designed to simplify scanning for new users. Their intuitive interfaces guide health workers through basic obstetric protocols step-by-step, ensuring consistent and reliable results.
This democratization of ultrasound use means POCUS for maternal health in rural Philippines can be integrated quickly into busy clinics, even when staff have limited prior imaging experience. It also makes scaling up ultrasound access across rural health networks far more achievable.
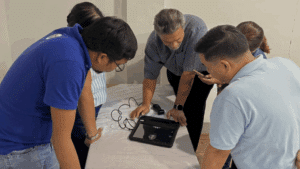
10. Building Sustainable Local Ultrasound Networks
Short-term POCUS training programs can spark change, but sustainable improvement comes from ongoing mentorship. The Catanduanes Ultrasound Fellowship is a prime example — offering graduates continuous education, tele-ultrasound supervision, and case reviews to keep skills sharp.
By creating a network of trained ultrasound “champions” across the province, the fellowship ensures knowledge is passed on, devices are actively used, and more providers are trained over time. This model can be replicated across other underserved areas, building a nationwide web of skilled providers ready to deliver safe, effective maternal care.
Conclusion: From Local Impact to National Transformation
POCUS for maternal health in rural Philippines is more than just a diagnostic tool — it’s a lifeline that is rewriting the story of maternal care in underserved communities. By detecting complications early, empowering local healthcare providers, and harnessing technology like ScanHub for real-time specialist support, we are closing the gap between rural and urban maternal health. The progress seen in provinces like Catanduanes shows what’s possible when innovation meets commitment. With sustained training, community engagement, and access to portable ultrasound technology, this impact can scale nationwide — ensuring no mother is left without the care she needs, no matter how remote her home may be.
Transform your practice with GUSI’s proven training programs:
- In-Person Courses – Master techniques with live instruction
- Fellowships – Become a POCUS expert through intensive training
- Online Courses – Learn anytime, anywhere with expert guidance
FAQs
1. Can POCUS replace traditional ultrasound in all cases?
No. POCUS is best used for screening and triage, with complex cases referred to specialists.
2. How long does it take to train a midwife in POCUS?
Basic obstetric POCUS training can be completed in 2–5 days, with ongoing mentorship recommended.
3. What is the role of ScanHub in maternal care?
It enables remote consultations and real-time specialist support for rural providers.
4. Can POCUS help with non-obstetric conditions?
Yes. POCUS is also used for cardiac, abdominal, and lung assessments in primary care.
5. How can donors support POCUS programs in the Philippines?
By funding devices, training, and mentorship programs for rural healthcare workers.
References
- Global Ultrasound Institute. POCUS Training Programs. https://globalultrasoundinstitute.com
-
- World Health Organization – Recommendations on Antenatal Care
- World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. Geneva: WHO, 2016.
- UNICEF Philippines. Maternal and newborn health in the Philippines. UNICEF, 2023.
- Moyo SR, et al. Point-of-care ultrasound in low-resource settings: a scoping review. Global Health Sci Pract. 2022.



