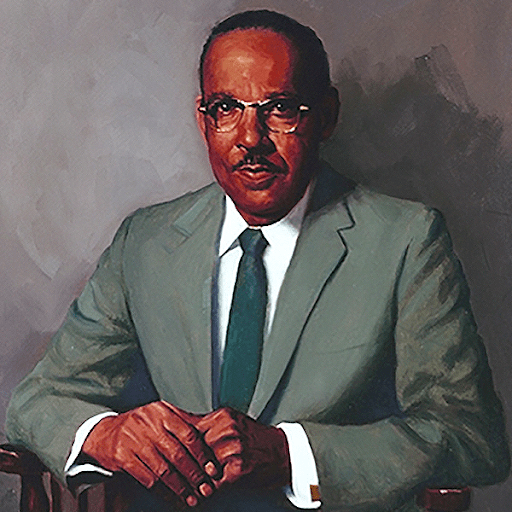
As we embark on February, a month of significance marked by Black History and American Heart Health, we are eager to illuminate the remarkable journey of Vivien Thomas. Born in Louisiana in 1910, Thomas’ story unfolds as an inspiring tale of resilience, determination, and unparalleled contributions to the field of cardiothoracic surgery given his circumstances.
Despite facing the setbacks of the Great Depression, Thomas experienced a loss of his college savings and the chance to fulfill his dream of attending college and medical school. However, he transformed adversity into an opportunity for innovation.
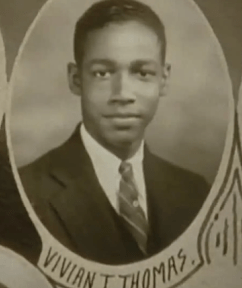
At the age of 20, Thomas’ journey took a pivotal turn when he joined Alfred Blalock, MD, as a laboratory assistant at Vanderbilt University. His innate talent and surgical dexterity were immediately evident, with his first day involving assisting in a surgical experiment on a dog. In short order, Thomas began conducting similar procedures independently, showcasing a natural aptitude for the intricacies of surgery.
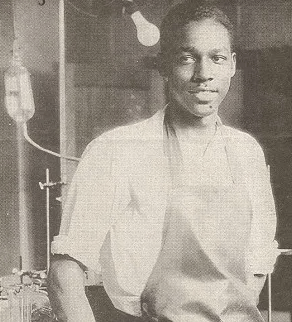
Blalock’s profound respect for Thomas transcended racial prejudices of the time. He declined a job offer that restricted him from hiring Thomas because of his race. By the age of 31, Thomas continued working with Dr. Blalock, who was now surgeon-in-chief at Johns Hopkins University.
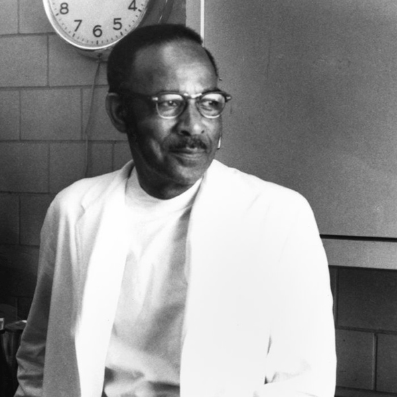
Despite facing racial and educational barriers, Thomas’s expertise contributed significantly to refining surgical techniques for the treatment of Tetralogy of Fallot, one of the causes of what was known as “blue baby” syndrome, that transformed the treatment of congenital heart defects. His relentless pursuit of excellence earned him the title of an “Instructor in Surgery” at Johns Hopkins, highlighting the impact of his work as a distinguished scientist and educator in the field of Cardiothoracic Surgery.
During his career, Thomas would later assume leadership roles in surgery departments across the United States, leaving an indelible mark on the education and training of numerous cardiac surgeons. He later went on to write an autobiography titled “Partners of the Heart” and was depicted in the 2004 biographical drama “Something the Lord Made.”
Today, the integration of ultrasonography into cardiac care has revolutionized diagnostics, allowing for non-invasive and precise visualization of the heart’s structure and function and early detection of congenital cardiac anomalies, such as tetralogy of Fallot, in-utero, and has become an integral part of prenatal care.
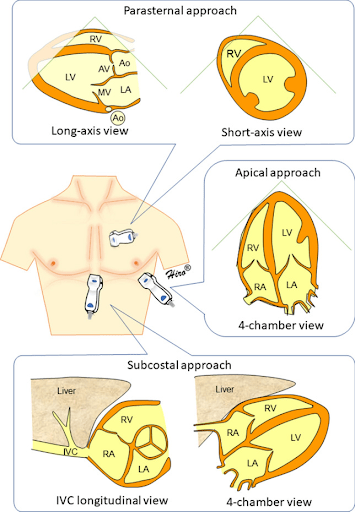
In contemporary primary care, the integration of echocardiography has become a transformative tool for focused cardiovascular assessments such as presence of pericardial effusion, qualitative assessment of ejection fraction, volume status, and evidence of right heart strain. This can help narrow the differential for causes of dyspnea and chest pain using the standard four views: Parasternal Long (PLAX), Parasternal Short (PSAX), Apical 4 Chamber (A4C), and Subxiphoid or Subcostal (SX, SC). In combination with lung ultrasonography, a limited echocardiogram can definitively distinguish between diagnoses such as COPD and CHF exacerbations in minutes.
As we reflect on the extraordinary contributions of Vivien Thomas and embrace the evolution of cardiac care through integration of echocardiography in primary care, we invite you to join us in commemorating Black History Month and American Heart Health Month. Together, let us honor the pioneers, celebrate diversity, and inspire innovation in the ongoing pursuit of cardiovascular health. Here’s to a healthier and more inclusive future for all.
 Case Study #1
Case Study #1
A 68-year-old male with a medical history relevant for systemic lupus erythematosus, antiphospholipid syndrome, chronic kidney disease, and atrial fibrillation presents in with acute onset abdominal pain that started abruptly after straining on the toilet. Upon arrival at the ED, the patient is experiencing severe pain in the mid abdomen that does not radiate but is pulsatile in nature. Vital: BP 90/50 mm Hg, HR: 120 bpm, RR: 20, afebrile, EKG is non-ischemic.
Differentials include bowel ischemia, perforated viscus, abdominal aorta aneurysm, small bowel obstruction, and nephrolithiasis. Bedside abdominal POCUS was performed on the abdominal aorta which demonstrated the following:
Point of Care Ultrasound performed at the bedside showed an abdominal aortic aneurysm in the process of rupturing with dissection of the vessel wall.
An abdominal aortic aneurysm (AAA) is characterized by an abnormal focal dilation (>3 cm) of the abdominal aorta. This is a relatively common condition and has the potential for significant morbidity and mortality. Most patients with AAA are asymptomatic but are identified through findings such as a pulsatile mass on physical examination. Risk factors include age, male sex, hypertension, and tobacco use. Because symptoms in association with a diagnosis of AAA increase the risk for rupture, symptoms that are not obviously attributable to another cause (eg, diverticulitis) should be presumed to be due to the aneurysm, until proven otherwise.
This patient was taken for emergent surgery and is recovering in the ICU under stable condition. Thanks to bedside POCUS, time for diagnosis was minimized, allowing for a prompt decision to intervene surgically.
 Case Study #2
Case Study #2
A 67- year- old male with a history of hypertension, diabetes, and a 42 pack-year smoking history presents to your urgent care with 3 days of worsening dyspnea. He admits it’s been “a few years” since he last saw a doctor. Vitals are: BP 144/94 mm Hg, HR: 98 bpm, RR: 22, afebrile, EKG is non-ischemic. Examination shows minimal pitting edema, some wheezes heard anteriorly and crackles posteriorly at the bases. The differential includes COPD exacerbation, CHF exacerbation, cardiac tamponade, pneumonia, PE, acute MI, and pneumothorax. Sonographic findings are shown below.
Studies have demonstrated that the use of POCUS for management of acute dyspnea can reduce time to diagnosis and expedite decision making, improving the accuracy of diagnosis by narrowing the differential.
You diagnose the patient with acute congestive heart failure and start him on diuretics and additional appropriate medications, order a comprehensive echo and refer him to cardiology as well as a follow up with his PCP.
(Cases contributed by Victor Vaz, MD)

Dr. Beryl Greywoode is an Attending Physician at Children’s Hospital of Philadelphia and an Assistant Professor at the University of Pennsylvania. She received her medical degree with honors from the University of Florida College of Medicine, where she founded the non-profit Project RAIN (Relieving Areas In Need). This initiative focuses on advancing sustainable health initiatives in Sierra Leone, her home country. She then completed her pediatric training in the Boston Combined Residency Program (Boston Children’s/Boston Medical Center) and pursued a Pediatric Infectious Disease Fellowship at Imperial Health in the United Kingdom, developing her clinical skills in both tropical health and international relief work. Though her global health work encompasses a broad range of issues, Dr. Greywoode has a keen interest in developing innovative solutions for low-resource settings that impact and augment health outcomes.
Dr. Greywoode is currently the Director for General Pediatrics Point of Care Ultrasound at the Children’s Hospital of Philadelphia, a program she developed from its inception. Through her ultrasound work, she has pioneered one of the first general pediatric inpatient ultrasound programs in the nation, training frontline hospitalists, residents, and medical students in the use of bedside ultrasound. She leads on a national level, influencing the use of ultrasound in the pediatric inpatient setting, serves on the leadership team for FUSEd (Focused Ultrasound in Education), an interdepartmental initiative for bedside education and research, and is a Course Director for CHOP’s Bedside Ultrasound Course, an internationally renowned training course in bedside ultrasound.
“Over the years I’ve been involved with a lot of ultrasound courses, yet it isn’t till teaching with GUSI that I’ve felt a cohesively supportive structure that will make a sustainable difference for the learner. POCUS is truly a transformative tool for both the one holding the probe and the patient at hand, yet the activation energy required for mastery of the skill can be seemingly steep. GUSI distills this process down into a form that can truly be called art, and particularly in accompanying the learner on their post-course journey, GUSI has answered the resounding question many learners ask of “what next?” I believe as the landscape of medicine and technology continually merge and change, GUSI will uphold a standard anyone pursuing knowledge of POCUS will want to adopt. As such, it is indeed a true honor to be part of the GUSI family and community of leaders dedicated to the mantra, “teach one, reach many.”
Dr. Beryl Greywoode
GUSI in the Community

In partnership with the American Friends of Jamaica and the JAHJAH Foundation, Dr. Bruno Vargas led basic OB POCUS training with handheld ultrasound in Kingston, Jamaica.
Dr. Mena Ramos led a team of 12 GUSI instructors and trained 65 clinicians from the University of Alabama across multiple specialties including family medicine, internal medicine, pediatrics and palliative care.
Dr. Laura Adam and Dr. Ian Thomas led an intro to POCUS for Primary Care hands on workshop for clinicians at the Eastern Connecticut Health Network.

Coming in March – GUSI’s scanOne™ App!
GUSI’s scanOne™ mobile app offers a fast, secure, HIPAA-compliant solution to anonymize and upload POCUS images from any ultrasound device. The scanOne app ensures accuracy and data integrity, to support sharing scans for QA and credentialing. Learn more.
“Of all the forms of inequality, injustice in health is the most shocking and the most inhuman because it often results in physical death”
–Dr Martin Luther King



