Webinar Summary: June 18, 2025 | Presented by Global Ultrasound Institute
Tuberculosis (TB) remains the world’s leading cause of death from an infectious disease, with over 10.8 million cases and 1.25 million deaths reported globally in 2024. In low-resource settings, early diagnosis continues to be a massive barrier to care. Could lung ultrasound (LUS) help fill that gap?![]()
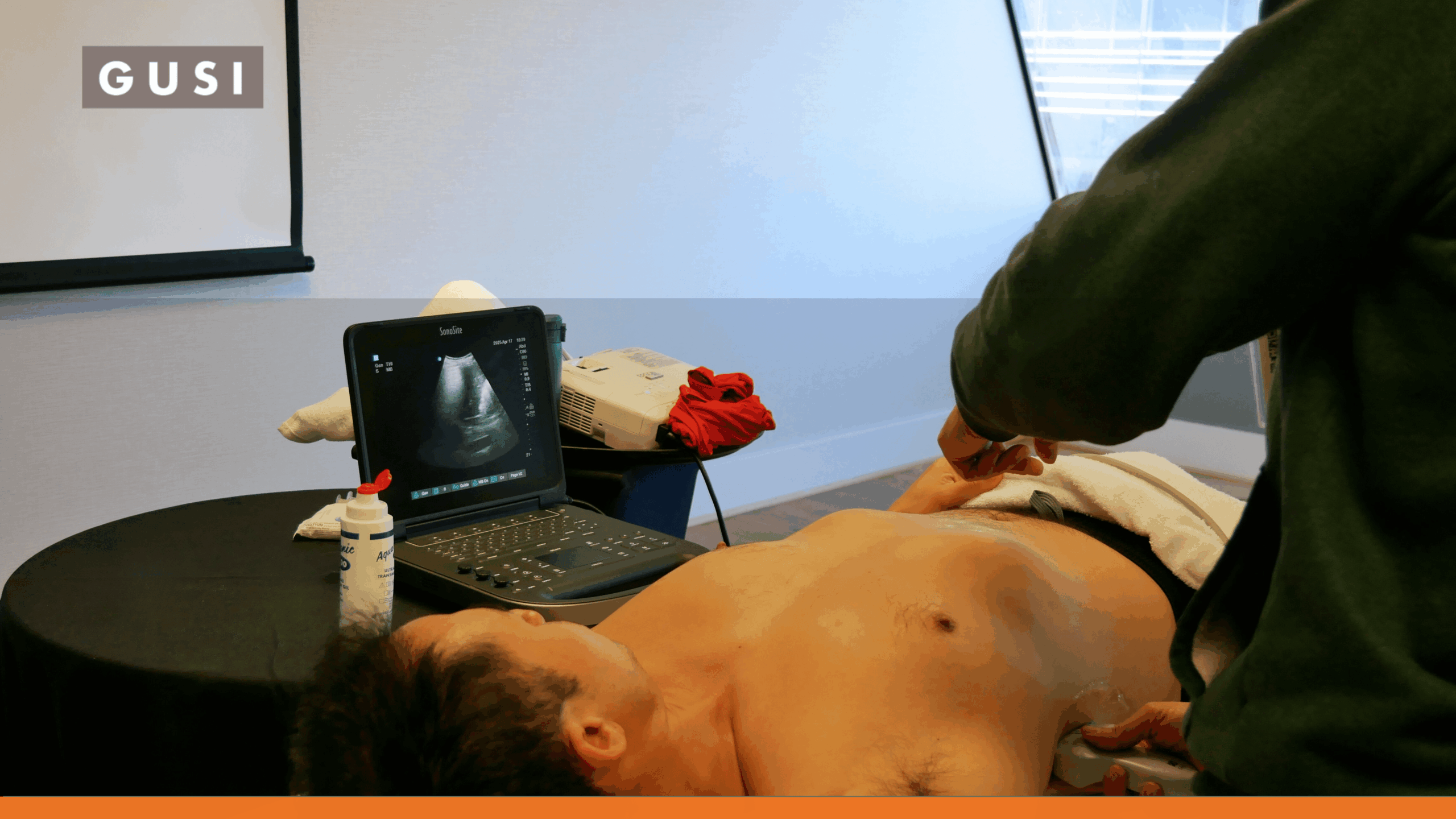
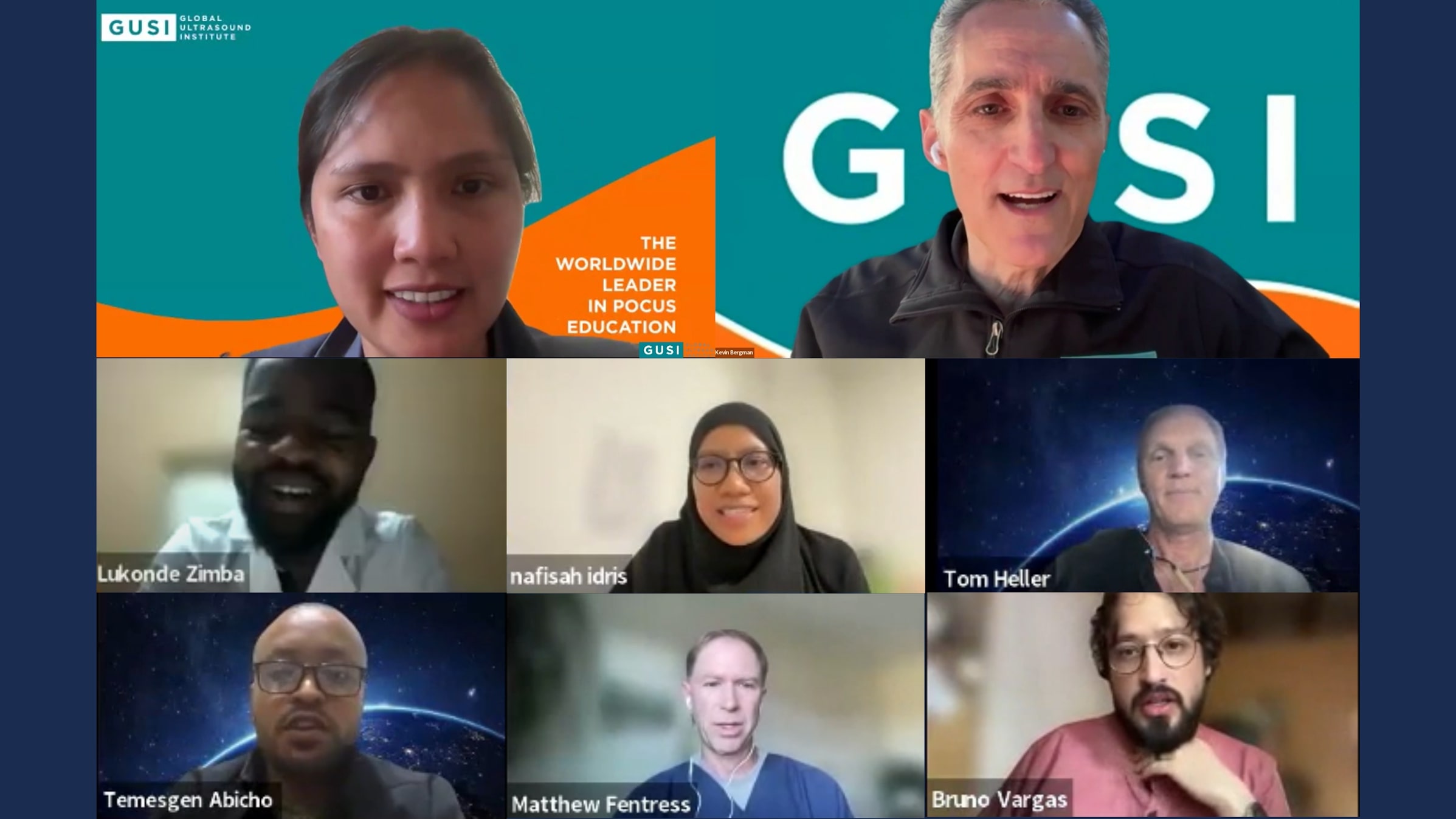
In this June 18 webinar, hosted by Global Ultrasound Institute (GUSI), Dr. Mena Ramos and Dr. Kevin Bergman brought together TB researchers, family physicians, emergency doctors, and ultrasound educators from six continents. This compelling discussion highlighted both the promise and the limitations of using Lung Ultrasound for Tuberculosis detection, triage, and clinical decision-making.
1. The Global Burden of TB and the Case for Lung Ultrasound for Tuberculosis
Dr. Lukonde Zimba (University of Zambia) opened the session with sobering statistics: Only 50% of people with TB are diagnosed or reported, and access to care remains highly inequitable. A scalable, low-cost tool like lung ultrasound may help detect more cases earlier, especially in resource-constrained areas.
TB disproportionately affects the most underprivileged populations. We need tools that meet people where they are.
2. What the Research Shows About Lung Ultrasound for Tuberculosis
Dr. Matthew Fentress (University of California, San Francisco) presented a systematic review of lung ultrasound findings in pulmonary TB, drawing from both older and recently published studies. He highlighted the diagnostic potential of specific LUS features:
- High Sensitivity for Subpleural Nodules and Consolidations (56% to 100%), especially when used as composite indicators
- Low Specificity for Composite Findings (44% to 66%), which limits standalone utility
- Inability to Visualize Cavitary Lesions in most cases, a known shortcoming of LUS
- AI Integration as a rapidly growing area of research that could scale access
He cautioned against generalizing LUS results without standardization, noting that no universally accepted set of criteria yet exists to define a positive scan for TB.
There is no standard definition yet of a positive ultrasound for TB. We need more research to define key lesion combinations.
3. Malaysia’s Frontline Study: Lung Zones That Matter Most in Lung Ultrasound for Tuberculosis
Dr. Nafisa Idris (Hospital Kuala Lumpur, Malaysia) shared results from a multi-center observational study involving 140 newly diagnosed pulmonary TB patients. The study excluded patients with prior TB or other chronic pulmonary conditions, focusing on correlating LUS findings with chest X-rays.
Key findings included:
- The R1A and R1B zones (right anterior upper chest) had the highest yield of positive LUS findings, aligning with known oxygenation and anatomical patterns of TB.
- Pleural irregularities were the most consistent finding, seen in 98% of patients.
- LUS showed greater sensitivity than chest X-ray in detecting early, peripheral disease, though the correlation with X-ray was moderate.
She described how this informed their emergency department triage process. Patients showing suspicious symptoms but inconclusive chest X-rays could be isolated and prioritized for TB workup using LUS findings as justification.
“In the ED, when X-rays show nothing but clinical suspicion is high, LUS gives us the evidence to isolate and protect.”
4. Global Clinical Applications of Lung Ultrasound for Tuberculosis: Case Stories from Mexico to Ethiopia
Panelists from three continents shared how LUS is applied in everyday clinical settings:
- Dr. Bruno Vargas (Partners in Health, Chiapas, Mexico) works in mountainous areas where patients must travel hours over dirt roads to access x-ray machines. He described LUS as a lifesaving extension of physical examination. In two illustrative cases, LUS findings such as pericardial effusion and pleural irregularity helped convince TB program officers to initiate treatment even before sputum results were available. He emphasized that LUS empowered frontline clinicians to act quickly.
“It’s not about replacing X-rays—it’s about getting patients diagnosed and treated when access is a barrier.”
- Dr. Temesgen Beyene Abicho (Bahir Dar University, Ethiopia) discussed how LUS plays a central role in emergency and critical care. In scenarios such as TB-related pericardial tamponade or pleural effusion, LUS is used for diagnosis, monitoring, and procedural guidance. He stressed how its portability and real-time capability made it indispensable for unstable patients, especially when radiology is far away or unavailable.
“From rapid diagnosis to guiding pericardiocentesis, point-of-care ultrasound is everything in the ED.”
- Dr. Tom Heller (Lighthouse Clinic, Malawi/Germany) highlighted the limitations and dangers of misclassification. His experience with HIV/TB co-infected patients emphasized the need for specificity. Subpleural consolidations—while common in TB—are also seen in bacterial pneumonia, lung malignancies, and embolism. He advocated for clearer definitions and more robust combinations of sonographic signs, possibly aided by AI, to build trust among TB officers and health ministries.
“Ultrasound isn’t one test. We need to define which signs matter—and in what combinations.”
5. The Role of AI in Scaling Lung Ultrasound for Tuberculosis
The panelists agreed: Artificial intelligence could help bridge the gap between LUS’s clinical potential and its practical application. A recent AI study from West Africa, shared during the webinar, demonstrated how algorithms trained on image patterns achieved the World Health Organization’s target sensitivity and specificity thresholds for non-sputum TB diagnosis.
However, panelists also expressed caution. AI must be interpretable, transparent, and clinically grounded. As Dr. Heller noted, “AI can’t be a black box—we need to understand what it’s doing and why.”
- “AI may be the bridge that allows minimally trained providers to use ultrasound effectively at scale.”
Still, the consensus was clear: LUS is not a replacement for chest X-ray or microbiological confirmation. It is a contextual, adjunct tool to aid decision-making, particularly where other diagnostics are inaccessible.
Quick Takeaways on Lung Ultrasound for Tuberculosis
- Lung ultrasound shows high sensitivity for TB-related subpleural lesions but lacks specificity
- Right upper lung zones (especially R1A/R1B) are critical scanning areas for PTB.
- AI-enhanced ultrasound could expand diagnostic reach in low-resource settings.
- Clear lesion definitions are essential for programmatic adoption.
- LUS is not a stand-alone test, but a useful adjunct for triage and clinical decision-making.
Conclusion: From Curiosity to Clinical Impact
This global dialogue revealed a shared vision: using point-of-care ultrasound to close diagnostic gaps in TB care. While many unanswered questions remain—particularly around specificity and standardization—the consensus is that lung ultrasound is worth exploring, researching, and integrating contextually.
“Pick up the probe. Start scanning. Learn from your patients. This is how we build better systems of care.”
—Dr. Bruno Vargas
As GUSI continues to convene clinicians and researchers worldwide, the next steps are clear: more research, more rigor, and more collaboration across borders. Lung ultrasound might not be the silver bullet for TB, but it is proving to be a sharp and scalable tool for global health.
Want to learn more about POCUS and tuberculosis?
Visit globalultrasoundinstitute.com to stay updated on upcoming webinars, publications, and POCUS training opportunities.
Want to Watch the Webinar Recording?
The full recording of the June 18 webinar, “Clinical Applications for Lung Ultrasound and Tuberculosis: Multi-Regional Perspectives,” is available now on our website.
▶️ Watch the recording here!
FAQs
1. Can lung ultrasound diagnose tuberculosis on its own?
No. Lung ultrasound is best used as an adjunct to clinical evaluation and other diagnostic tools like chest X-rays and sputum testing.
2. What lung zones should be prioritized for scanning in Tuberculosis?
The right upper anterior zones (R1A and R1B) show the highest frequency of abnormalities in confirmed PTB cases.
3. How does AI help with ultrasound in Tuberculosis?
AI can improve image interpretation and help standardize findings, making it easier for minimally trained providers to use Lung ultrasound.
4. Is lung ultrasound better than chest X-ray?
Lung ultrasound may detect peripheral lesions missed by chest X-ray, but it cannot visualize central or cavitary lesions well.
5. What are the biggest limitations of Lung ultrasound in tuberculosis care?
Low specificity, operator dependency, and the lack of standardized definitions for tuberculosis-related findings.
Have feedback or questions?
Tag us on social or email us at [email protected]. Let’s keep the global conversation going.
References
-
WHO Global TB Report, 2024
-
Fentress M. et al., Systematic Review on lung ultrasound in tuberculosis, 2021
-
Idris N. et al., Malaysian PTB Lung Ultrasound Study, 2025 (presented)