An overview of the integration of point-of-care-ultrasound (POCUS) into primary care.
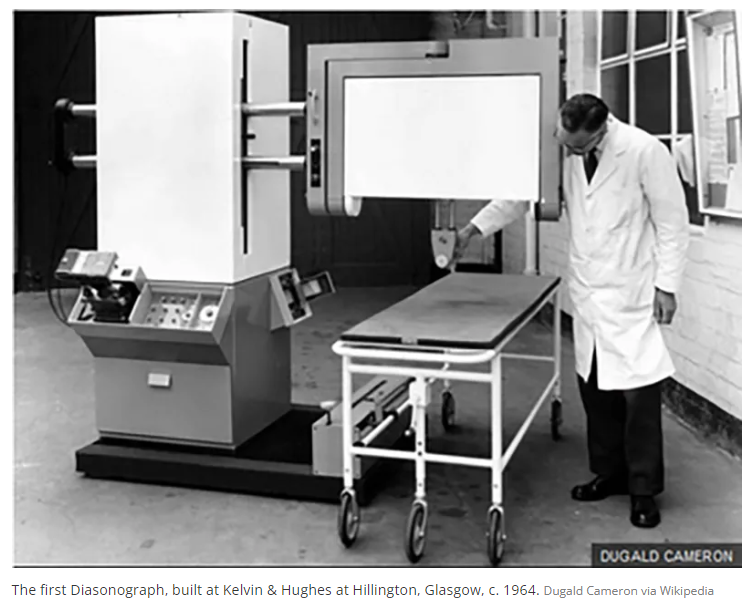
Initially, ultrasound technology was cumbersome and expensive, limiting its use to radiologists who utilized it primarily for diagnostic imaging in dedicated radiology departments. As the first adopters, radiologists set the foundational standards for its use, focusing on high-quality imaging to support accurate diagnoses.
As ultrasound technology evolved through the 1970s and 1980s, it began to gain traction among obstetricians and gynecologists. This specialty recognized the value of ultrasound for fetal monitoring and assessments during pregnancy. The portable nature of the newer ultrasound models allowed obstetricians to conduct real-time assessments, significantly enhancing prenatal care by providing immediate insights into fetal health and development.
“You have to know the past to understand the present.” – Carl Sagan
By the late 1990s and early 2000s, emergency medicine physicians started to adopt POCUS (Point of Care Ultrasound) as a crucial tool for rapid bedside diagnostics, particularly in trauma cases and other urgent care scenarios. The ability to make swift, accurate assessments in the emergency room transformed patient care, enabling faster decision-making that was critical in acute situations.
 In the last two decades, we have witnessed an advent of even more advanced technological innovations. Ultrasound equipment has become more portable, affordable, and user-friendly. This evolution has expanded its use beyond traditional hospital settings and specialized departments, making POCUS an invaluable diagnostic tool at the bedside of patients in various medical fields. Today, it is increasingly utilized in primary care, where general practitioners employ it to enhance the scope of their diagnostics and patient management. This shift has democratized the use of ultrasound technology, allowing for broader applications in healthcare and improving access to essential diagnostic tools in a variety of settings.
In the last two decades, we have witnessed an advent of even more advanced technological innovations. Ultrasound equipment has become more portable, affordable, and user-friendly. This evolution has expanded its use beyond traditional hospital settings and specialized departments, making POCUS an invaluable diagnostic tool at the bedside of patients in various medical fields. Today, it is increasingly utilized in primary care, where general practitioners employ it to enhance the scope of their diagnostics and patient management. This shift has democratized the use of ultrasound technology, allowing for broader applications in healthcare and improving access to essential diagnostic tools in a variety of settings.
Recent endorsements by major healthcare bodies highlight the growing recognition of POCUS’s value in primary care.
As advocated by the World Organization of Family Doctors (WONCA), the integration of POCUS can fundamentally alter diagnostic processes, improving the efficiency and accuracy of primary care services globally. (Poppleton et al, 2025)
Empirical studies underscore the profound impact of POCUS on healthcare delivery. Research indicates that POCUS can substantially reduce wait times and the overall cost of care. A notable study published in The American Journal of Medicine reveals that the application of POCUS in primary care not only decreases unnecessary referrals but also reduces the need for expensive diagnostic procedures, thereby offering substantial cost savings.
Furthermore, the concept of “number needed to scan” (NNS) emerges as a critical metric in evaluating the efficacy of POCUS. In a 2021 study by Amini et al, NNS was defined as the number of POCUS exams needed to be performed to “change one management plan, prevent one adverse outcome from a procedure, or catch one missed diagnosis.” The study found the average NNS for a POCUS exam ranged between 2-5. Comparing this to statins given for 5 years for heart disease prevention, the number needed to treat (NNT) to prevent a non-fatal heart attack, save a life, or prevent a stroke are 35, 83, and 125 respectively. (Hodgson et al 2011)
Since the technology and use for ultrasound has changed dramatically since standards were first established, there has similarly been development in what is considered an adequate scan to answer a specific clinical question (POCUS), different from standards for comprehensive scans. There are many areas of consensus for common POCUS scans, and new techniques and applications are being developed.
Barriers to POCUS Integration
(Nathanson et al 2023)
- Training and Education: One of the primary barriers to widespread POCUS adoption is the need for substantial training. Many primary care physicians and other specialists may not have received adequate ultrasound training during their formal education. This gap can lead to underutilization or incorrect application of POCUS, which could potentially compromise patient care.
- Cost and Accessibility: Despite becoming more affordable over time, the initial cost of ultrasound equipment can still be a barrier for smaller practices or low-resource settings. Additionally, the maintenance and updating of ultrasound technology can add to the financial burden.
- Quality Control and Standardization: There is a lack of standardized protocols and quality control measures across different regions and institutions. This variability can affect the reliability of ultrasound examinations and the confidence of practitioners in using this technology.
- Regulatory and Reimbursement Issues: In some regions, there may be regulatory hurdles or insufficient reimbursement policies for ultrasound procedures performed by primary care providers, which discourages its use.
- Cultural Resistance: Some practitioners may be resistant to adopting new technologies or changing traditional diagnostic processes, particularly if they are not familiar with ultrasound technology. Additionally, there may be interdepartmental difficulties as well.
As we continue to explore the benefits and challenges associated with the adoption of POCUS in primary care, it is clear that its potential to revolutionize patient care is immense. Check out our free webinar library for strategies on integrating POCUS into your practice and residency.
Resources
- Hodgson R. Number-needed-to-treat analysis: An explanation using antipsychotic trials in schizophrenia. Advances in Psychiatric Treatment. Jan 2011. 17(1) DOI:10.1192/apt.bp.108.005959
- Thavendiranathan P. Primary prevention of cardiovascular disease with statin therapy. Arch Int Med. 2006; 166: 2307-13.
- CTT Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomized trials of statins. Lancet. 2005; 366: 1267-1278.
- Ridker et al. Rosuvastatin to prevent vascular events in men and women with elevated c-reactive protein. NEJM. 2008; 359(21): 2195-2207. http://www.ncbi.nlm.nih.gov/pubmed/20167359
- Nathanson, R., Williams, J. P., Gupta, N. (2023). Current use and barriers to point-of-care ultrasound in primary care: A national survey of VA medical centers. The American Journal of Medicine, 136(6), 592-595.e2. https://doi.org/10.1016/j.amjmed.2023.01.038
- Poppleton A, Tsukagoshi S, Vinker S, et al. World Organization of National Colleges, Academies and Academic Associations of General Practitioners and Family Physicians (WONCA) Europe position paper on the use of point-of-care ultrasound (POCUS) in primary care. Primary Health Care Research & Development. 2024;25:e21. doi:10.1017/S1463423624000112