Newsletters
Navigating Cold and Flu Season: The Power of POCUS in Respiratory Diagnosis | Dec 2023 Newsletter

As the crisp autumn air settles, giving way to winter, we find ourselves entering the cold and flu season—a time when respiratory illnesses are at the forefront of health concerns. In the midst of this challenging period, staying informed and leveraging our diagnostic toolbox becomes paramount. That’s why we are excited to bring you the latest insights on leveraging Point-of-Care Ultrasound (POCUS) in the diagnosis of COVID-19, pneumonias, and other respiratory conditions.
In this edition of our newsletter, we’ll explore the role of POCUS as a game-changer in the field of respiratory medicine. POCUS offers a rapid, non-invasive, and highly accurate approach to diagnosing a range of respiratory illnesses, enabling healthcare professionals to make timely and informed decisions.
Auscultation has stood as the keystone of the lung physical exam and, more broadly, as the symbol of a clinician. Recent systematic reviews and meta-analyses have compared lung auscultation with other modalities commonly used in detecting lung pathology, such as chest x-ray and ultrasound. They demonstrated that although we use lung auscultation as a screening tool, its sensitivity alone may not make it the best tool to function in that role.
A recent publication by Marini et al. in 2021 summarized literature comparing lung ultrasound (LUS) and chest x-ray. It demonstrates similar specificities but much superior sensitivities without the risk of radiation.

A significant portion of our current knowledge in lung ultrasound stems from Dr. Daniel Lichtenstein’s landmark paper in 1998. The paper discussed the use of artifacts to differentiate between pulmonary edema and COPD. Since that time some of the nomenclature was later redefined by Dr. Lichtenstein and what was then described as “roughly horizontal parallel reverberating lines” is now called A-lines and what was then called comet-tail artifact is now referred to as B-lines (defined as stretching below 16cm of depth). Additionally comet-tails artifact is now referred to as Z-lines and are defined distinct from B-lines and have no clinical significance:
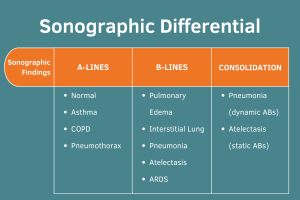
Learning the “ABCs” of the lung can be helpful for interpretation of sonographic findings.
-
“A” or A-lines can be regarded as a normal lung artifact, but can also be seen in pneumothorax, asthma exacerbation, and COPD exacerbations in the right clinical context.
-
“B” or B-lines can be seen in pneumonia, pulmonary edema, interstitial lung disease, atelectasis, and acute respiratory distress syndrome (ARDS).
-
“C” or Consolidations are commonly seen in pneumonia and atelectasis and can be distinguished by clinical context and presence of static vs. dynamic air bronchograms (ABs).
Check out the sonographic images.



A recent paper in the Journal of Clinical Ultrasound in 2022 summarized various sonographic findings of COVID in the lungs and other organs. The findings also encompass methods for conducting a sonographic examination of the lungs (see below). Other studies have shown that these findings can reflect both the duration of infection and the severity of the disease. Another recent systematic review and meta-analysis demonstrated that the findings of COVID-19 interstitial pneumonia on ultrasound have high diagnostic agreement with CT scans. It can be considered an equally accurate alternative to CT in situations where molecular tests are not available.
Common findings in COVID-19 patients include:
-
Irregular/Thickened Pleural Lines
-
Small Subpleural Consolidations
-
B-Lines (bilateral)

As we navigate the challenges of cold and flu season, expanding our diagnostic toolbox and arming ourselves with knowledge become instrumental in ensuring the well-being of our communities. So before you order your next chest x-ray, take five minutes to perform a brief lung ultrasound exam and compare your findings to the x-ray results!

 Case Study #1
Case Study #1
A 63-year-old male without significant medical history presented to the emergency department (ED) with dry cough and intermittent chest discomfort. He had undergone a normal serologic workup along with an unremarkable chest x-ray and electrocardiogram (EKG). His vital signs were normal. He was soon to be discharged from the ED with a presumed viral URI when along came the bored POCUS team who offered a cardiopulmonary examination.

His lung scan did not reveal any significant abnormalities apart from some small, trivial subpleural consolidations. There was no pulmonary edema, no pleural effusions, and no significant consolidations or air bronchograms.
When asked to lie flat for the cardiac exam, he noted worsening chest discomfort. Upon obtaining the initial Parasternal Long Axis (PLAX) view, all eyes in the room grew wide in surprise.

Here you can see a significant pericardial effusion in PLAX and Subxiphoid views with concerns for early tamponade. This was communicated with the cardiology team who promptly drained 400cc of serosanguinous fluid. Ultimately there was no obvious source for this effusion. Since this experience, I always make sure to take at least a quick peek at the heart in respiratory cases where lung ultrasound is unrevealing.
 Case Study #2
Case Study #2
A 68-year-old male with known congestive heart failure (CHF) was seen for a new cough, increased dyspnea upon exertion, increased lower extremity edema and low-grade fever. Physical exam revealed bibasilar crackles, bilateral lower extremity edema, and weight gain above dry weight. A working diagnosis of acute decompensated heart failure exacerbation was made.



Bedside ultrasound revealed the expected diffuse B-lines in the bilateral posterior lower lung zones; however, it also found a consolidation in the left lower lung, seen here with the shred sign as well as a small pleural effusion. Therefore the patient was additionally treated for community-acquired pneumonia, which might not have been addressed without the use of point-of-care ultrasound (POCUS)!
——-
To contribute valuable learning cases and propose future POCUS topics for our newsletters, please email [email protected] with the subject line “Newsletter.”
Currently, he collaborates with Arc Health, offering healthcare services to tribal communities in rural New Mexico. Bedside ultrasound has emerged as an indispensable diagnostic tool in this setting, especially considering the challenges many patients face in accessing the nearest hospital for imaging needs.
Dr. Schoneich’s professional interests encompass global health and health equity, an exploration of the broader structural sources of diseases, and the education and application of POCUS to diminish barriers to care in resource-limited primary care settings.
Beyond his professional endeavors, Sebastian enjoys cycling, daydreaming about the seaside, and spending quality time with family and friends at a beer garden.
GUSI in the Community

In collaboration with Butterfly Network and supported by a generous grant from the Bill and Melinda Gates Foundation, GUSI has expanded its OB POCUS training to encompass eight counties in Kenya. This represents a significant step in advancing healthcare practices within the region.
The palpable enthusiasm displayed by healthcare professionals during the training was truly inspiring. Their eagerness to incorporate POCUS into their practice speaks volumes about the potential positive impact on maternal health and fetal outcomes. This initiative is a testament to the collective commitment to advancing healthcare standards and improving the overall well-being of the community.

GUSI recently concluded another successful Point-of-Care Ultrasound (POCUS) training at the Touro College of Osteopathic Medicine (TOUROCOM). Participants left with enhanced skills and confidence after engaging in hands-on scanning sessions and high-yield lectures.
Thank you to our global POCUS community of inspiring healthcare professionals who strive daily to improve patient care with Point-of-Care Ultrasound. As we approach the end of 2023, we cannot express enough gratitude to the GUSI team of POCUS experts, who make it possible to transform health systems one patient at a time. This past year, we witnessed the largest scale deployment of POCUS training among midwives in Kenya, the use of POCUS at the forefront to triage patients in conflict zones in Ukraine, and many other places. The transformative impact of Point-of-Care Ultrasound is palpable. The trust built every time a provider picks up the probe to show a patient why they may be having pain or coughing, the confidence built every time a provider picks up the probe to narrow their differential diagnosis, the culture built by putting the patient at the center of decision-making – these are at the heart of what we do. It is an honor for our organization to play a role in the transformative journey of POCUS in healthcare.
With appreciation and gratitude, from Kevin, Mena, and The GUSI Team
Sign up for GUSI’s e-newsletter and updates here

 Case Study #1
Case Study #1