Newsletters
POCUS vs. Traditional Sonography: Perspectives from a Sonographer turned PA | Oct 2024 Newsletter

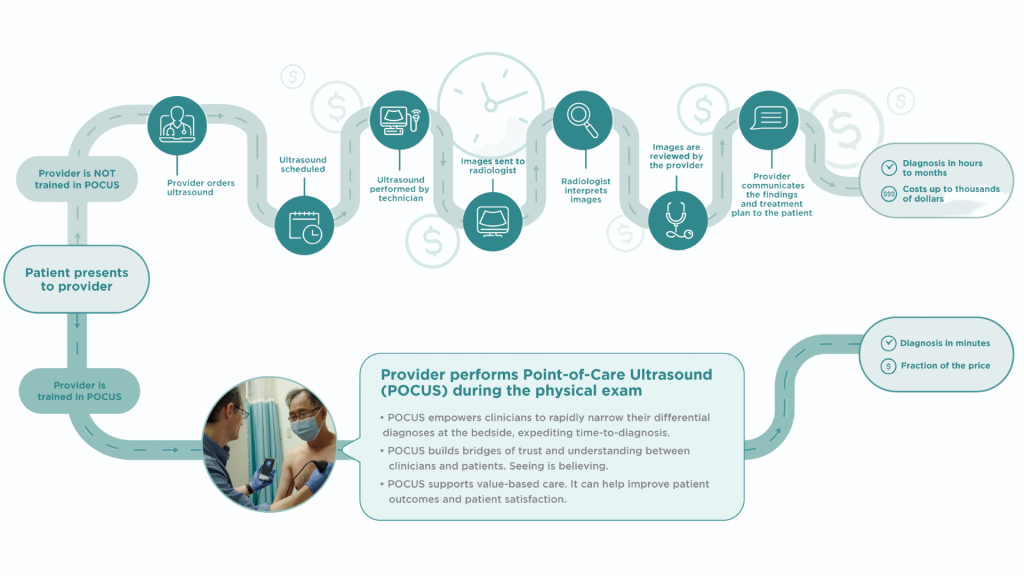
The increased accessibility of portable devices have made the practice of POCUS much more ubiquitous in a range of clinical settings beyond emergency medicine and critical care. POCUS, however, has been described since the 1990’s when laptop sized devices were introduced which allowed clinician’s to perform bedside ultrasound at the “point-of-care” to answer a focused sonographic question that could impact immediate decision making at the bedside. POCUS describes a streamlined clinical workflow whereby the clinician is performing a focused ultrasound at the “point-of-care”, most commonly with a cart-based (laptop sized) or handheld device.
This month’s newsletter will focus on how POCUS differs from traditional sonography by sharing the first hand experience of Agnes Lovell, a sonographer turned PA.
“As a sonographer turned PA-C, October is a special month to me because it’s medical ultrasound awareness month (MUAM) AND it’s PA week from October 6-12th. I worked as a vascular sonographer for seven years prior to PA school, spending an entire career mastering the fine art of ultrasound. Like many others, the pandemic impacted me in profound ways and I decided I wanted a bigger piece of the pie and to grow into being a provider. So, to PA school I went. In my PA training, I’ve had the opportunity to use POCUS in the OR to vein harvest for open heart surgery, in the emergency department for FAST exams and ophthalmic emergencies, and for many types of procedures in my elective IR rotation. Now, as a newly graduated PA-C I’m looking forward to utilizing POCUS in my practice in internal medicine.
Reforming my approach from a sonographer to a POCUS user has been a challenging shift in perspective. Sonographers are methodical, precise, intense, and admittedly take more than a little pride in being the experts wielding the transducers and knowing more about your insides than you ever will. Imagine spending years learning how to coax a vertebral artery into revealing its secrets and then POCUS comes along and it’s like someone handed out a polaroid camera and says “forget the intricate stuff, snap a picture and move on.” For a sonographer, it’s like telling a Michelin star chef to microwave a burrito. It’s doable, and microwave burritos can be delicious and filling, but there’s this existential dread in the process. It was disorienting at first, I had to let go of the gorgeous diagnostic imaging to be formally read by radiologists and surgeons to focus on the more practical purpose of POCUS exams.
Diagnostic sonography is different from POCUS in a lot of ways. Diagnostic ultrasound (DUS) is like your friend who spends too much time analyzing every detail of a movie when you ask them if it was good or not. DUS is thorough. You want accuracy? You get accuracy. Bring a book because it might take a while. DUS is usually performed by a trained sonographer or a radiologist and uses cart based equipment. These cart based machines have multiple transducers and intricate settings, each transducer costs thousands of dollars. The diagnostic sonographers are highly trained, often with a minimum of two years of full time ultrasound education. It’s usually performed in an imaging department with a dedicated space : hopefully ergonomically designed in a nice dark room. These exams are performed to a credentialing body’s specifications with required images and data gathered. The preliminary report is written by the sonographer, and the final report is written by the interpreting physician. As you can imagine, this takes anywhere from a few hours to several days to get a final report. A lot of time and energy is spent in obtaining DUS. It’s separate from the patient’s care in a sense, as it’s just one piece of the puzzle and oftentimes “clinical correlation is advised.
In comparison, POCUS is a frontline tool used bedside, during patient care, in real time. It’s like your no nonsense friend who you turn to when you need an answer quickly and efficiently. These are usually performed with handheld or laptop based devices with one, maybe two transducers available. It’s done on a gurney, or in the field, maybe under bright fluorescent lights and sometimes requires awkward body positioning to perform. POCUS is much more practical and answers specific clinical questions. Since it’s being performed by the clinician with the information and the questions at hand, it’s raw and wildly useful. There’s something undeniably satisfying about being able to swoop in, do a quick scan, and actually make a clinical decision. If we’re still yearning for those picture perfect images, we can get a DUS afterwards for our fix.”

Agnes Lovell PA-C
University of Washington, PA Program
Seattle, Washington
To summarize, the primary differences between Point-of-Care Ultrasound (POCUS) and traditional ultrasound lie in their application, implementation, and the context in which they are used:
|
POCUS |
Traditional Ultrasound |
|
|
Location |
Bedside |
Radiology Department or Sonography Center |
|
Availability |
More Accessible and Immediate |
Usually hospital based or sonography center |
|
Scope |
Focused Clinical Question |
Comprehensive |
|
Equipment |
Cart Based, Handheld Devices |
Larger, Multi-Probe, Devices |
|
Operator |
Clinician (ie. Doctor, Nurse, PA, Midwife) |
Sonographer, Radiologist |
|
Speed |
Minutes, Hours |
Hours, Days, Months |
References:
- [1] “Point-of-care ultrasound in obstetrics and gynecology.” in Arch Gynecol Obstet. 2021 Feb 8; 303(4):871-876
- [2] “Role of echocardiography in clinical hypertension.” in Clin Hypertens. 2015 Jun 17; 21:9
