POCUS: a Pluripotent tool for a Pluripotent specialty
What if I told you there was a technology that could drastically reduce time to diagnosis, lower healthcare system costs while generating value during patient visits, engage patients more deeply with their care, improve health equity and help family doctors find their work more meaningful and satisfying?
What if I told you this technology already exists, but we aren’t doing enough to lower barriers and facilitate widespread use in Family Medicine?
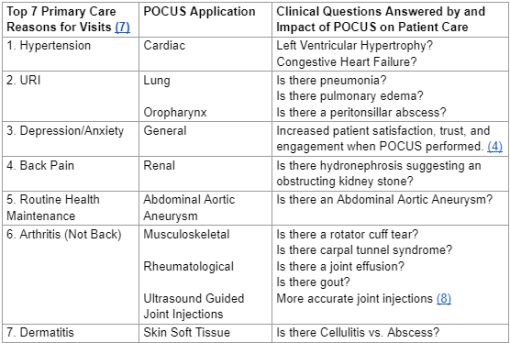
Enter Point of Care Ultrasound (POCUS) – ultrasounds performed by clinicians during patient encounters to answer focused clinical questions. POCUS has already taken obstetrics by storm, and improved flow in Emergency Departments worldwide. With the new ACGME guidelines released in July 2023 requiring POCUS in Family Medicine residency training (1), POCUS is poised to have an even more transformative impact in the world of Family Medicine.
Many family doctors – including myself – chose our specialty because we value the importance of meeting our patients where they are at, want to involve patients deeply in their care, and understand the importance of continuity relationships. Yet we are faced with a fragmented healthcare system and – along with our patients – witness the financial costs and emotional tolls of disjointed care:
The patient who we sent to the Emergency Department because we were worried about a Deep Venous Thrombosis, but who didn’t go because they were worried about copays.
The patient who suffered through our ineffective attempts to treat heartburn while waiting weeks to get the ultrasound diagnosis of gallstones.
The uninsured patient who was so excited when we helped them quit smoking, but who couldn’t afford an Abdominal Aortic Aneurysm screening out of pocket and ended up in the ED with a rupture.
The pregnant patient who comes to her first prenatal visit with bleeding, wondering if her baby is ok.
POCUS gives family doctors the capacity to change these patients’ stories, and so many more. When we can make diagnoses in the moment, we save our patients time and money, deepen their trust and engagement, and make our own work vastly more meaningful. POCUS decreases costs from unnecessary additional testing saving patients thousands per visit in a community Emergency Department (2). It improves patient care and decreases length of stay through faster and more accurate diagnoses of common presentations such as shortness of breath(3). Moreover, POCUS can add financial value to patient visits if billed as a procedure, and also helps to facilitate in-office procedures like injections. It increases patient satisfaction, trust, engagement, and perceived quality of care (4). It reduces burnout by actually making our work more meaningful (5). And because it has the most impact for patients who face the greatest barriers to accessing care, POCUS it improves health equity (6). For Family Medicine doctors practicing in inpatient, emergency, and peripartum settings, POCUS also has myriad applications in these arenas. In short, POCUS allows family doctors – no matter their practice setting – to be the most effective clinicians they can be.
Like any new technology, POCUS faces barriers to adoption. Despite the many benefits, fewer than 10% primary care physicians have POCUS integrated into workflows (9). Common barriers include lack of access to and protected time for longitudinal training, and access to machines (10). Health systems need to facilitate training opportunities and machine access, as well as creating clinician schedules and billing strategies that promote integration of POCUS into patient visits.
Fortunately, thanks to POCUS champions at all levels, change is already starting to occur. As a family medicine doctor working in a safety net hospital, I’ve seen countless patients’ faces light up as I hand the probe to them and say “show me where it hurts”, and seen how this simple act changes the course of their care. And as the founder and educational director of Global Ultrasound Institute (GUSI), I’ve seen countless clinicians’ faces light up as they see how this lifesaving technology will transform their medical practice.
As family physicians, we have already committed to being the first stop for our patients’ needs. We are already a procedure-oriented hands-on specialty and were among the first physicians to use ultrasound at the point of care in the 1990’s (11). POCUS has the potential to help Family Medicine physicians reclaim the essence of our specialty, while transforming our care. I hope you’ll join me in working towards a future where all Family Medicine physicians have POCUS at their fingertips.

Mena Ramos, MD
Dr. Ramos is a Family Physician, Co-Founder of Global Ultrasound Institute (GUSI), a leader in point of care ultrasound education and training worldwide. www.globalultrasoundinstitute.com. She is a global advocate for the use of POCUS among frontline healthcare providers. The team at GUSI develops scalable POCUS solutions for health systems through longitudinal mentorship, a web-based learning platform and app, cloud-based quality assurance, machine learning tools, and in person training. Dr. Ramos completed her FM residency at the Contra Costa Family Medicine Residency Program, co-authored the 2016 AAFP National POCUS Guidelines, and is an Assistant Professor at the UCSF Department of Family and Community Medicine.
Reference :
https://issuu.com/cafamilydocs/docs/cfpq_-_winter_2023-2024_vol_74_no_4 (Pages 14-15)
Sources:
(1)https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint290D_POCUS.pdf
(2)https://onlinelibrary.wiley.com/doi/abs/10.1002/jum.14910
(3)https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10017566/#:~:text=Time%20to%20diagnosis%20
(4)https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8214303/
(5)https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8918294
(6)https://www.jabfm.org/content/jabfp/34/4/853.full.pdf
(7)https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6234945/
(8)https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3324992
(9)https://www.jabfm.org/content/34/4/859
(10)https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9508689
(11)https://pubmed.ncbi.nlm.nih.gov/7810467/


