E-newsletters
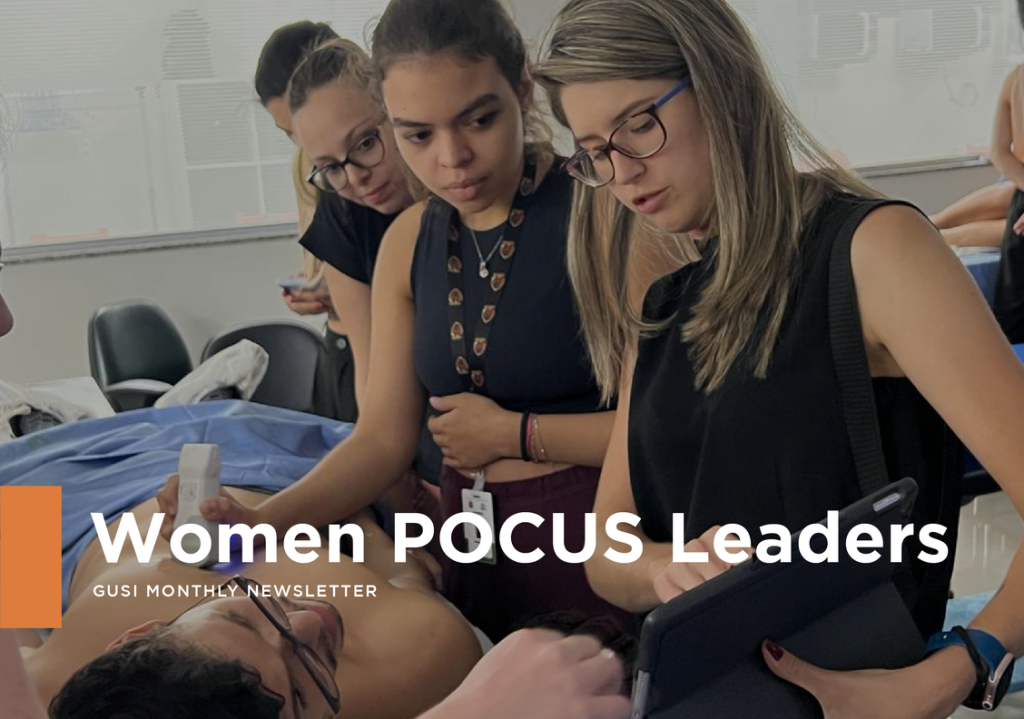
March 2023: Women POCUS Leaders
In 1849, Dr. Elizabeth Blackwell became the first woman to graduate from a medical school in the United States. Since then, women physicians, nurses, advanced practice practitioners have made tremendous contributions to the field of medicine. In 1864, Dr. Rebecca Lee Crumpler became the first Black woman in the US to earn a medical degree and in 1889, Dr. Susan La Flesche Picotte became the first Native American woman to become a doctor.
Women have played an integral role in the advancement of POCUS education. Since the 1960’s, Point-of-Care Ultrasound (POCUS) has expanded beyond solely obstetric applications. In the 1980’s the use of ultrasound as a bedside tool, known as POCUS was largely developed in emergency medicine to get immediate answers in potentially life threatening conditions. However, the applications for POCUS are not solely limited to emergency medicine. In the last 20 years, we have seen an expansion of the use of POCUS in hospital medicine, critical care, ambulatory medicine, and primary care. This expansion coupled with rapid technological development in the form of smaller, portable, durable, cost effective devices has catalyzed a revolution in bedside medicine to incorporate insonation as the 5th pillar of the physical exam.
In celebration of Women’s History month, we asked women POCUS leaders and GUSI instructors across various medical specialties what they love most about Point-of-Care Ultrasound.
|
|
Dr. Sally Graglia (Emergency Medicine) Director Med Student POCUS Education, University of California San Francisco “I love POCUS because it brings me closer to the patient. I love POCUS because it makes me more confident in my diagnosis.” |
|
|
Dr. Puja Dalal (Family Medicine) APD, Ultrasound Program Director, Novant Family Medicine Residency “I love POCUS because it allows for increased access to medical care, especially for vulnerable populations.”
|
|
|
Dr. Smita Sinha (Obstetrics and Family Medicine) AAFP Foundation Family Medicine Leads Emerging Leader Institute Scholar “What I love about POCUS is the ability to make an immediate diagnosis without the patient having to make a separate appointment in the imaging department, not to mention scheduling delays especially in the primary care setting.” |
|
|
Dr. Keasha Guerrier (Family Medicine, Health Systems Administration) Chair Family Medicine LIJ Valley Stream Hospital Quality Director, Department of Family Medicine Board of Governors, Northwell Health Director ”I love POCUS because my patients get answers in real time, it saves the health system money, and it makes my practice so much more rewarding.” |
|
|
Carrie Hayes PA-C, RDMS, RVT (Sonographer and APP) Former Director of Ultrasound, RAD-AID Inteleos POCUS Ambassador to USA “As a clinical and procedural provider, POCUS is a quick, painless and effective tool, allowing timely assessment and management of key clinical questions, as well as real time guidance of both diagnostic and therapeutic interventions.”
|
|
|
Dr Kirstin Weerdenburg (Pediatrics) Co-Director Pediatric POCUS, IWH Health Halifax, Nova Scotia ”I love being able to connect with patients and caregivers at the bedside on what I am or am not seeing with POCUS, which I think improves understanding, compliance and satisfaction.”
|
|
|
Dr. Sahar Ahmad (Critical Care) Director of Ultrasound Education, Renaissance School of Medicine at Stony Brook University “Mastering POCUS brings you closer to the patient. Unlike ordering CT scans and X-rays which are done from your computer, POCUS is a technique that brings you to the patient’s bedside. This skill when used as an extension of the physical exam and history taking allows for us to discover the needs of patients and have accelerated sophisticated conversations with consultants- all for the betterment of patient care. It feels an inherent aspect of doctoring well, certainly in my field.” |
|
|
Dr. Tanping Wong (Internal Medicine) POCUS Fellowship Program Director Cornell Weill Medical School “To love POCUS…. Is to See human physiology Be with others that want to change the world, That knows no boundaries. Bound by a shared love….. POCUS.” |

Case Study #1
A 22-year-old female patient presents to your clinic with vaginal spotting, abdominal cramping, and is 3 weeks late on her period. She had a positive home pregnancy test done earlier today. Her last pregnancy ended in a spontaneous abortion. She has no history of sexually transmitted diseases or ectopic pregnancies. The patient’s vital signs are normal and her abdominal exam is soft. The resident performs the ultrasound below.

DX. Threatened Abortion
You find a fetal pole and measure a fetal heart rate of 150 bpm. You take a quick look behind the uterus and at the adnexa and find no obvious signs of ectopic pregnancy. A FAST exam was negative for intra abdominal free fluid.
To rule out an ectopic pregnancy, you must rule in an intrauterine pregnancy because the negative-predictive value for ectopic pregnancy when an intrauterine pregnancy is identified is 99.96% (Stein et al. 2010)
Remember that in order to confirm an intrauterine pregnancy it is not only necessary to see the gestational sac, but also to visualize either the yolk sac, the fetal pole, or a heartbeat. Also, remember not to use color Doppler routinely to measure the FHR during the first trimester because of the theoretical risk of harming the fetus
And don´t forget to reassure your patient that bleeding occurs in up to 27% of pregnancies (Hasan et al, 2010)
Case Study #2
You are in a primary care rural clinic in the Sierra of Mexico. The closest hospital is a 5 hour drive away along difficult roads. A 32-year-old female presents to you with chronic lower abdominal pain and dyspareunia. She had 2 previous pregnancies, with the last one being preterm 3 years ago. She walked 2 hours to get to your clinic and tells you that due to inaccessibility and lack of money, she hasn’t been able to get herself properly checked. She has seen other healthcare providers and received multiple treatments for pain management but never had an ultrasound performed.
As part of your exam, you decide to perform an abdominal ultrasound and see the following:
From the images, it appears as though she has two uteri.
This is an example of a Mullerian duct anomaly (MDA). The septate uterus is the most common MDA followed by the bicornuate, arcuate and didelphys being the second least common. (Rezai et al, 2015)
The images above suggest a bicornuate or a didelphys uterus. You obtain patient consent to perform a speculum where you are able to visualize two cervixes as well as a thin longitudinal vaginal septum. When having a patient with Didelphys uterus it is also important to look for any renal anomalies and obstructed hemivagina as they can be part of the Herlyn Werner -Wunderlich syndrome (Passos and Britto) In this case, both kidneys were present. It is important to state that 2D ultrasound has limited use in correctly differentiating MDA, but 3D ultrasound and MRI can help without having to pursue more invasive methods like hysteroscopy or laparoscopy. (Rezai et al, 2015)
Your ultrasound correctly identified the anomaly after which the patient was referred to a specialist to confirm the diagnosis of a didelphys uterus.
Cases Contributed by Dr. Bruno Vargas (Partners In Health, Chiapas, Mexico)
Smita Sinha Kumar, MD graduated from Kasturba Medical College, Manipal, India with a Masters’ degree in Obstetrics and Gynecology. After graduation she joined as a faculty at Manipal Teaching Hospital in Pokhara, Nepal. She then joined the teaching university hospital in rural Punjab, India where she established the first low-cost fertility service and brought minimally invasive surgery to the area. She established a residency training program in ObGyn and taught medical students for several years.
She then received a scholarship to get an MBA in Healthcare at Clarkson University in New York where she graduated with the Joseph Finkelstein Award 2020 for academic excellence and cross-cultural understanding. She worked as a Project Manager in upstate NY before being drawn back to patient care where she decided to pursue the specialty of family medicine. She is a PGY2 at Institute for Family Health, Kingston, NY. In 2022, Dr. Sinha and was awarded the AAFP Foundation Family Medicine Emerging Leadership Institute Scholarship for her work in reproductive health. Recognizing the value POCUS can bring to primary care, she is championing POCUS in her residency and is working with the Global Ultrasound Institute team to boost POCUS in primary care. She believes in advocating for her patients and was recently in Capitol Hill lobbying Congress to support grant funding to support teaching programs that serve resource constrained communities.
GUSI’s Upcoming POCUS Events
GUSI’s POCUS for Primary Care in San Francisco April 13-14, 2023 is SOLD OUT. However, there are more opportunities to learn Point-of-Care Ultrasound right around the corner. Stay tuned, our next POCUS for Primary Care course will be in San Francisco on October 5-6, 2023.
GUSI on the Move!
GUSI in Brazil teaching a hands-on intro to POCUS workshop for medical students and residents in São Paolo, Brazil. The course was met with great enthusiasm from students and teachers alike!

Dr. Mena Cayetana Ramos, Dr. Werlley de Almeida Januzzi, and Dr. Renata Moreira Marques Passos facilitating POCUS training for 70 medical students and residents March 21-22, 2023 at Instituto de Assistência Médica ao Servidor Público Estadual (IAMSPE).
We would love to come teach at your institution! Click here to contact us.

GUSI’s Global Outreach
In response to Tropical Cyclone Freddy and the devastating impact in Malawi and Mozambique, Global Ultrasound Institute is supporting clinicians in both countries with FREE access to POCUS education. If you know of any clinicians practicing in either country who would benefit, feel free to forward this link.
GUSI Offers New POCUS Courses
GUSI was excited to participate at the American Physical Therapy Association meeting in San Diego last February! We believe that Point-of-Care Ultrasound can improve the quality of bedside care provided by healthcare providers of various specialties.

Check out GUSI’s new POCUS course for physical therapists!
And stay tuned for the release of GUSI’s OBGYN POCUS Essentials and POCUS for Critical Care courses!
GUSI’s Quality Assurance
Ultrasound scan review is fundamental to any credentialing process. The only way to build confidence and competency in POCUS is by doing many practice scans and having timely expert feedback on those scans.
If you need help with QA for your leaders or yourself, you can count on our expert team.
We have made Scan Review more accessible than ever!
Best wishes,
Kevin, Mena, & the GUSI Education Team
Sign up for GUSI’s e-newsletter and updates here.