E-newsletters
April 2022: GUSI – GUSI And The Art Of Medical Education
“Medicine is learned by the bedside and not in the classroom. Let not your conceptions of disease come from the words heard in the lecture room or read from the book. See and then reason and compare and control. But see first.” William Osler

Fildes, L. (1891)The Doctor [Oil on canvas].
Source.
This month’s newsletter is dedicated to healthcare education and the role that POCUS has in training current and future healthcare workers. POCUS is an important diagnostic tool, and becoming proficient in its use is empowering.
At GUSI, we are excited that POCUS has become an integrated part of many specialties and many clinicians. We wholeheartedly agree with Dr. Osler, who said that clinical medicine is best learned through seeing, and POCUS is the best way to extend the clinician’s eyes from outside of the body, and go within. This belief drives all of our educational programming – including in person courses, online learning modules, and one on one coaching. Ultimately, POCUS allows the clinician to honor the tradition of bedside clinical medicine, while still allowing for the use of real time innovative technology and synthesis of point of care clinical data.
We hope this issue will help to highlight the current trends and status of POCUS education and skill development for students and trainees.

CASE STUDY #1
You are a senior Internal Medicine Resident seeing patients in Continuity Clinic. The last patient of the day is complaining of a painful, warm, and swollen right leg after a long car trip. He is 60 years old and has a history of diabetes. During the clinic visit, he does remark that actually both legs do appear somewhat swollen from baseline, but he is more concerned about the right leg. He is otherwise stable and feels well.
You consider your differential diagnosis and decide this patient needs to be ruled out for DVT. Should this patient go to the Emergency Department, an outpatient radiology facility, or can you perform a point of care ultrasound?
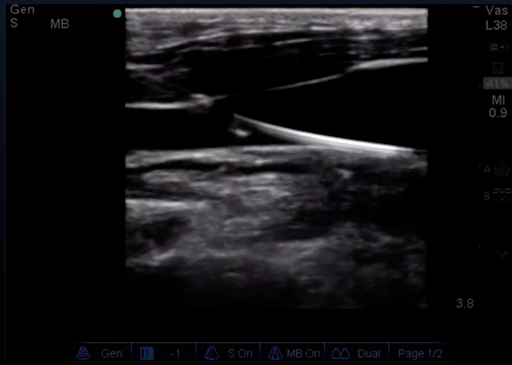
DVT in the Popliteal Vein
Your supervising attending frequently uses POCUS in the clinic and together you decide to perform the ultrasound. Providers proficient in POCUS can successfully perform evaluation for DVT at the bedside in the clinic, decreasing time to diagnosis and treatment. This can save time, money, and potential harm to the patient from delay in care. [Article]
CASE STUDY #2
You are a critical care resident working an overnight shift. The sickest patient of the night is an 80 year old woman with sepsis who is developing metabolic acidosis and refractory hypotension. You and your attending decide that this patient will require a central line to be placed for access and to administer pressors. You expertly place a right sided internal jugular triple lumen catheter. During the procedure you consider if POCUS could be used instead of chest XR for catheter placement confirmation and to rule out pneumothorax.
Confirmation of wire placement (Source)
You and your attending discuss the following article and consider POCUS makes it possible to confirm central line catheter placement quicker than with traditional chest XR. [Article]
You also discuss the process of using agitated saline to help with central line placement confirmation. Learn more here.
CASE STUDY #3
In your orthopedic rotation, a 90 year old patient presents to the Emergency Department with severe hip pain after a fall. After radiology imaging, it is determined that the patient has sustained a right side femoral neck fracture. The patient is scheduled to go to the Operating Room the next morning, but in the meantime you wish to address her pain. Part of the multimodal pain control strategy includes performing a femoral nerve block through administration of a long acting anesthetic such as bupivacaine. [Article]
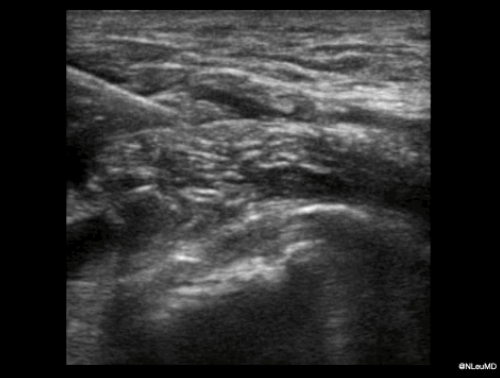
POCUS Image provided by Dr. Nathaniel Leu
Learn more about the process of administering the block here.
Faculty Spotlight
Parth Rali, MD is an Associate Professor in Division of Thoracic Medicine and Surgery at Lewis Katz School of Medicine at Temple University Hospital, Philadelphia. Dr Rali is the Director of Systemwide Pulmonary Embolism Response Team (PERT) Program and also the Chair of National PERT consortium protocol committee. His area of interest and expertise includes pulmonary embolism, cardiac critical care, and point of care ultrasound focused on acute RV failure. Dr Rali has more than 60 peer reviewed publications, serves on the conference programming committee (pulmonary circulation) for American Thoracic Society. Dr Rali recently has become part of CHEST COVID-19 VTE guidelines committee. Dr Rali serves as Principal Investigator and Sub PI in more than 30 clinical trials with special focus on VTE trials.
POCUS Training is for Everyone
We are so thankful to everyone who joined us for our April Flagship In-Person course, POCUS for Primary Care in San Francisco – which was sold out!

This course was our biggest course to date, featuring 50 participants and 10 POCUS instructors. Participants represented a broad range of specialties from family medicine, internal medicine, community medicine, hospitalist medicine, and pediatrics – from practice settings including outpatient, clinic, urgent care, emergency medicine, and critical care. They also represented physician faculty, physician program directors, fellows, residents, medical students, physician assistants, and nurse practitioners.

This was a 2 day course with short lectures interspersed with longer scanning sessions, with a machine to learner ratio of 3:1. This provided for maximal time to learn and develop POCUS skills, within a clinical framework provided by the instructors. POCUS training included the abdomen, cardiac, pulmonary, gallbladder, renal, aorta, DVT, and procedures.
Day 2 was special because it provided more advanced training for musculoskeletal ultrasound and. We were joined by instructors Dr. Ryan Petering, Rachel Erickson, Christy Prill and John Mitchell, experts on musculoskeletal and sports medicine from OHSU. This is the beginning of more expansive educational offerings that GUSI will provide on MSK.

Stay tuned for the next course POCUS for Primary Care, October 20-21, 2022 in San Francisco!
GUSI on the Move
Webinars
- Next Webinar: Starting a POCUS Program in your Residency: Panel Discussion and Q&A, May 24 at 12pm EDT/9am PDT. Register for it here.
- Dr. Paul Bornemann is also the lead author for the textbook Ultrasound for Primary Care. Check it out here.
- Stay tuned for future webinars on: Making the Business Case for a POCUS program, Overcoming Common Obstacles in Developing a POCUS Program, POCUS Fellowships, and POCUS in FQHCs.
Health Equity Residency Exchange (HERE)
The Health Equity Research Exchange (HERE) program is the latest way that GUSI is living up to its promise to share POCUS with medical professionals from around the world.
We are now recruiting volunteers to support POCUS education in resource limited settings. Contact us at [email protected]
Additionally – for every resident who signs up to learn with GUSI, we will extend a full scholarship to a resident practicing in a low- or moderate-income country. Learn more and sign up to participate here.
Check out GUSI on Social Media
Learn more about POCUS for should exams and assessment of shoulder injuries and pain:
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6595130/
- https://www.acep.org/emultrasound/newsroom/apr2021/pocus-for-shoulder-pain-in-the-emergency-department/
GUSI in the community

Best wishes,
Kevin, Mena, & the GUSI Education Team
Sign up for GUSI’s e-newsletter and updates here.

