E-newsletters
August 2022: GUSI – Healthcare Inequalities
Racism and inequality have unfortunately been entwined with medicine since the earliest days, and many examples, both historic and contemporary, abound. One such example is the infamy around Dr. James Marion Sims, regarded as the founder of OB/GYN.
The last few years of the COVID-19 pandemic have also revealed socioeconomic inequalities which also play out in healthcare. The pandemic has provided time for reflection, allowing those in medicine an opportunity to address this. An article like this publication from JAMA highlights the need to rethink racism, rather than race, as a risk factor for disease in patients.
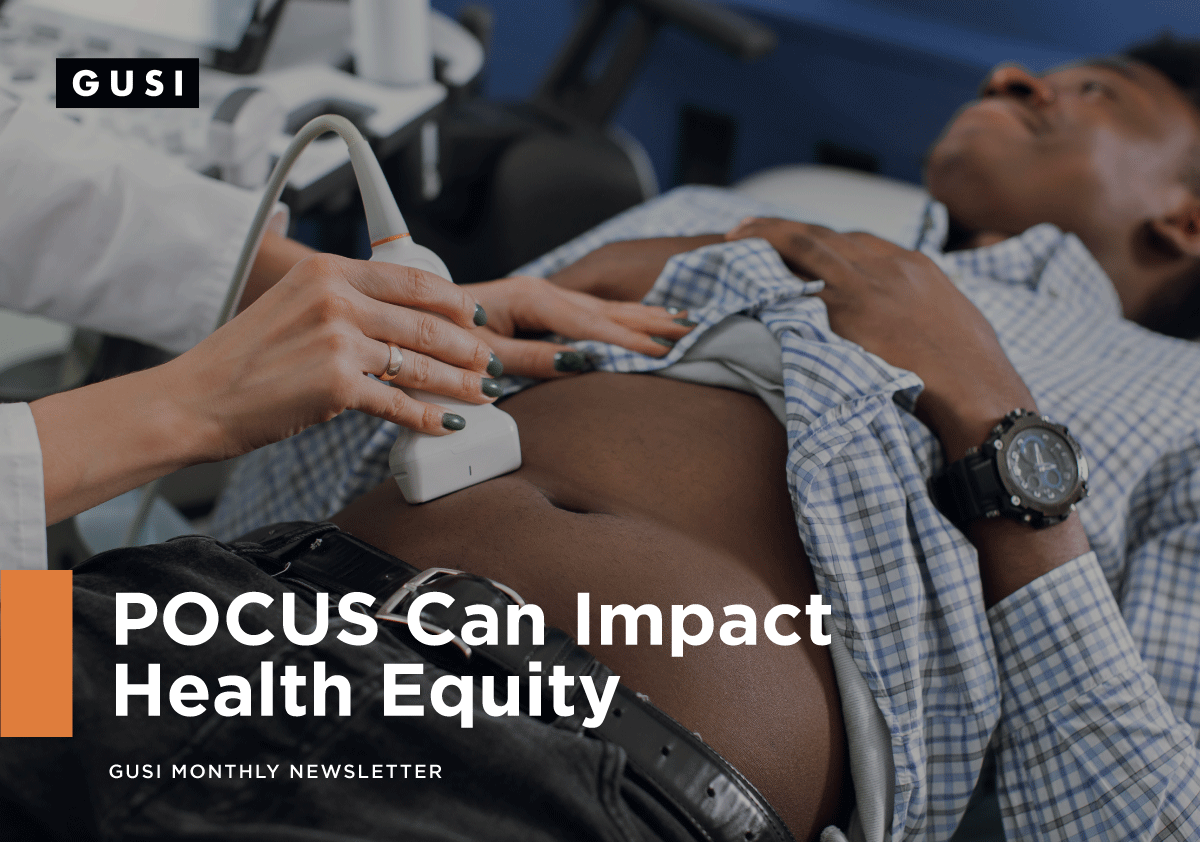
At GUSI, we know acknowledging healthcare inequalities in medicine requires open and honest dialogue. We also know that teaching POCUS can help break down systemic and structural barriers of racism in medicine through two strategies:
-
To empower clinicians to provide real-time and point-of-care medicine within marginalized communities.
- To create a more racial-ethnic inclusive ultrasound community.
We have a lot to learn and we know there will be missteps but we hope that spreading the knowledge of POCUS to all corners of the world will allow clinicians to provide the same excellent standard of healthcare to all, and help to reduce healthcare inequalities.
Case Study #1
A 60-year-old Spanish-speaking woman with housing insecurities presents to your walk-in clinic for 2 months after experiencing floaters in her right eye. She intermittently has mild pain in the eye, along with nausea and headache. She has a history of glaucoma and is supposed to be using “eye drops” that were previously prescribed in Mexico. She can’t recall the name of her eye drops. Additionally, these medications were recently stolen, along with her other possessions. She has been unable to follow up with her doctor appointments because of mobility issues related to chronic pain and challenges accessing public transportation.
Your patient also has a history of diabetes, hypertension, and previous strokes. As part of your workup, you get a visual acuity that is 20/200 in the R eye and 20/50 on the L eye. The eye pressures are normal in both eyes. Given that your differential includes retinal detachment, you also elect to do a POCUS ocular ultrasound.
The POCUS exam confirms your diagnosis of retinal detachment. Based upon this, you are able to expedite ophthalmology follow-up and restart the patient on her eye drops.
Learn more about the use of POCUS in the management of eye complaints through this article, a prospective diagnostic study of 225 patients. The authors found that POCUS had an overall sensitivity of 96.9% and specificity of 88.1% for the diagnosis of retinal detachment, 81.9% sensitivity and 82.3% specificity for vitreous hemorrhage, and 42.5% sensitivity and 96.0% specificity for vitreous detachment. This really makes POCUS a valuable tool for the evaluation of eye complaints.
Case Study #2
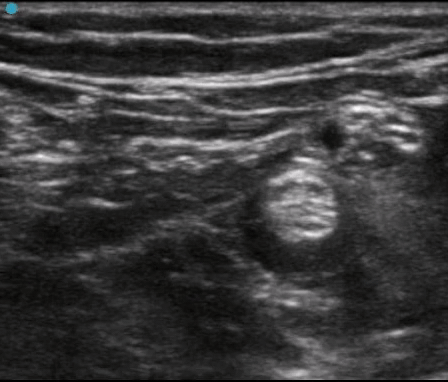
A 5-year-old African American boy is brought to your pediatric clinic after 1 week of abdominal pain. His mother had taken him to the emergency department 3 days ago. They waited several hours to be seen, and ultimately the boy was diagnosed with constipation and advised to use Miralax daily. Today he appears withdrawn and burrows his face into his mother’s side when you enter the exam room. When coaxed, he points to his periumbilical area when you ask him for the location of his pain. Based on the persistent abdominal pain and difficulty in getting an accurate exam on the patient, you perform a POCUS ultrasound of the appendix.

You are able to diagnose appendicitis. Based on this finding and labs that show an elevated white blood cell count, you transfer the patient to the children’s hospital for management of acute appendicitis. Learn more about pediatric POCUS abdominal exams here.
There is research that has shown that racism and ethnic disparities contribute to delays in the diagnosis of appendicitis in pediatric patients, which can have a significant negative impact on morbidity and mortality. We are also starting to learn that there are even racial and ethnic differences, where black and brown children are less likely to have appropriate diagnostic imaging performed, even when clinically indicated. Access to POCUS reduces these barriers and can help address these inequalities.
Case Study #3
A 30-year-old woman who works at a grocery store presents by ambulance to the emergency department after a twisting injury to the ankle and subsequent inability to walk. She tripped over a box while she was stocking shelves. You diagnose a bimalleolar fracture without any signs of dislocation, neurovascular compromise, or skin tenting. After successfully splinting the patient’s ankle, you try to perform an ambulation trial with crutches. However, she experiences severe pain despite Tylenol and Motrin. You consider prescribing narcotics, but she informs you that she currently is stabilized on buprenorphine and does not want to take any potential medication that could lead to dependence. You decide to perform a popliteal sciatic nerve block to provide multimodal pain control.
Learn more on how to perform popliteal sciatic nerve block here and here.
Medication Assisted Treatment (MAT) is the use of medications, in combination with counseling and behavioral therapies, which has revolutionized how we approach patients who have Opioid Use Disorder (OUD). Buprenorphine has especially been helpful to transition patients away from opioids and to better health. Learn more here.
POCUS Training is for Everyone
Registration is now open for our flagship POCUS Training Course taking place on October 20-21, 2022! Take advantage of our Early Bird Registration rates through Aug 20, 2022.

This highly acclaimed two-day in-person course combines high-yield lectures and hands-on scanning sessions, and also offers CME. Most of all, the emphasis is on maximizing POCUS scanning time through low instructor: learner and learner: ultrasound ratios.
Check out some highlights from our in-person course last April:
GUSI In Person POCUS SF from Global Ultrasound Institute
Faculty Spotlight
Dr. Puja Dalal is a trailblazer in POCUS and family medicine. She was initially introduced to POCUS in medical school where USCSOM had one of the first longitudinal ultrasound curricula for students. After completing her residency in Family Medicine at Swedish First Hill, she completed a Primary Care Ultrasound Fellowship at Prisma Health/USCSOM in Columbia, SC. She is now faculty at Novant Family Medicine Residency in North Carolina as the Ultrasound Program Director and Assistant Program Director. She is passionate about teaching primary care physicians POCUS to help expand much-needed access to medical care in low-resource settings.
GUSI on the Move
GUSI traveled to Little Rock, Arkansas to teach Introduction to POCUS for Primary Care! We would love to come to teach at your institution!
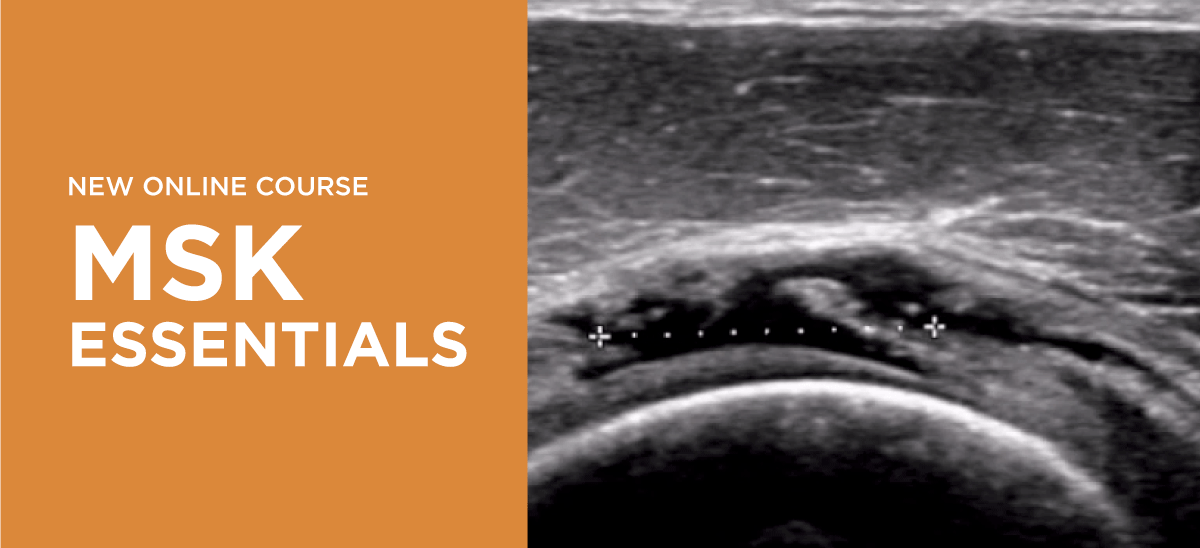
We’ve released our new MSK Essentials Course. Learn more about it here.
GUSI in the Community

Check out Mena having a great time teaching Intro to OB Ultrasound for rural nurse midwives in Maasin, Southern Leyte, in the Philippines.
Best wishes,
Kevin, Mena, & the GUSI Education Team
Sign up for GUSI’s e-newsletter and updates here.

