E-newsletters
January 2023: POCUS in 2023: New ACGME Requirements and more!
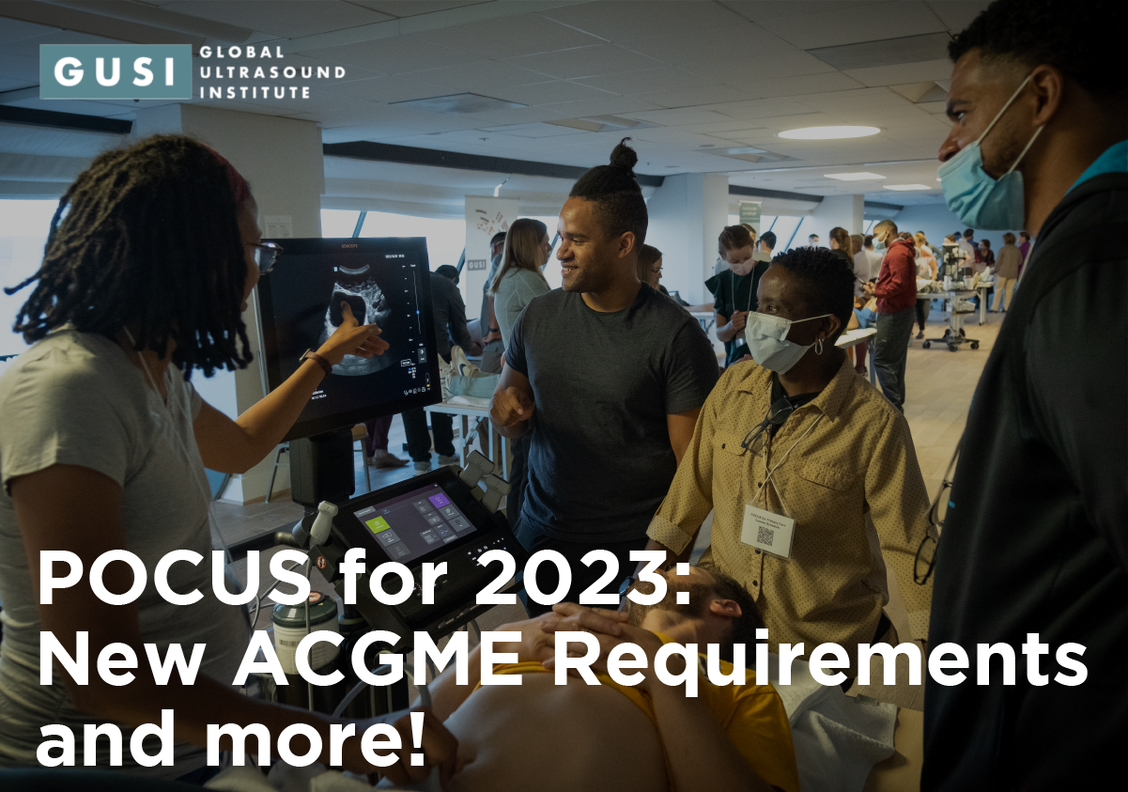
The beginning of 2023 is a wonderful opportunity to build upon the momentum of last year’s accomplishments and reflect on the barriers that kept us from achieving our goals. Whether it is Integrating POCUS into your clinical practice, learning new POCUS skills, or establishing POCUS training in your residency, POCUS integration in 2023 is both timely and achievable! Our mission at GUSI is to offer the most complete desktop solution to integrate POCUS into postgraduate education and training.
“The Secret of Making Progress is to Get Started” — Mark Twain
Reflection
It has been over 200 years since Laennec published de L’auscultation Mediate where he introduced the stethoscope as a diagnostic tool in Paris. During the last 200 years, there has been no other rapid and portable diagnostic tool like the ultrasound available to clinicians to help us answer basic diagnostic questions. With ultrasound, we now have a tool that bridges two chapters in the history of medicine. The chapter where doctors spent more time at the bedside using the tools at their disposal to gather information and establish rapport with patients and the new chapter of high data technology and rapid data transfer. Ultrasound allows us to benefit from both of these worlds to ultimately provide better care for our patients.

Opportunity & Timing
2023 is already shaping up to be a big year with the launch of the new ACGME POCUS training requirements in family medicine.
In 2022, the majority of US Medical Schools now have POCUS integrated into the curriculum. We are seeing similar trends in other specialties such as internal medicine, critical care, pediatrics, anesthesia, and general surgery. For now, with POCUS integrated into undergraduate medical education, POCUS integrated into ABFM knowledge assessments, POCUS clinical experience being required in family medicine training, all arrows are pointing in the same direction: POCUS as standard of care in bedside evaluation.
“IV.C.3.t).(1) Residents should have experience in using point-of-care ultrasound in clinical care.”
Preparation
Given the tremendous opportunity and timing, how can we best prepare to integrate POCUS into our practice in 2023?
1. Incorporate POCUS in the clinical setting for the management of your patients
How do you currently incorporate POCUS in your clinical practice and while taking care of patients?
Over the last ten years, we have seen an explosion of growth in realizing the potential for POCUS to revolutionize bedside medicine by providing real time clinical data to help guide management of patients. In a recent NEJM article that reviews this important technology and states, “POCUS is an inclusive term”, which the authors mean to say that POCUS has application in almost every specialty, and a broad array of clinical encounters.

2. Getting your reps in by practicing getting the most optimal views

How often do you practice doing POCUS?
Are you building your portfolio of de-identified images?
With focus and practice, the various aspects of POCUS are all attainable – image acquisition, accurate interpretation, and integration in the immediate clinical setting through medical decision making. This involves understanding the basics of the different types of ultrasound probes, the optimal way to position the patient, and various methods by which to navigate differences in each patient’s anatomy. Becoming expert in accurate interpretations of the images acquired requires performing POCUS exams regularly to understand the variety of ways “normal” images can present, and to help identify the abnormal.
3. Use Point of Care Ultrasound (POCUS) during procedures
Do you regularly use POCUS while performing procedures?
It is without question that ultrasound improves patient safety. In this article from the intensive care literature, ultrasound guided thoracentesis and paracentesis led to both safer and more cost effective care. For clinicians who learned how to perform a central line using landmark guidance alone who subsequently learned to perform the procedure with ultrasound guidance, learning to perform the same procedure with ultrasound guidance not only safety but confidence.
Check out this article for 5 simple procedures for starting out using POCUS in procedures by American Academy of Family Physicians.
4. Get Hands-On Experience at an In Person POCUS Conference
How do you keep up to date on POCUS knowledge and training?
GUSI can help guide and train any practitioner, regardless of their comfort level with POCUS. We have curriculums available for both individuals, and for groups of learners such as residency programs.
Check out our faculty who cross many specialties and have taught around the world with us.
5. How do you Implement and Manage a POCUS Curriculum in your practice or Residency Program?”
Did you know that as part of the GUSI desktop solution, learners and faculty can track course completion, questions and scans by type?
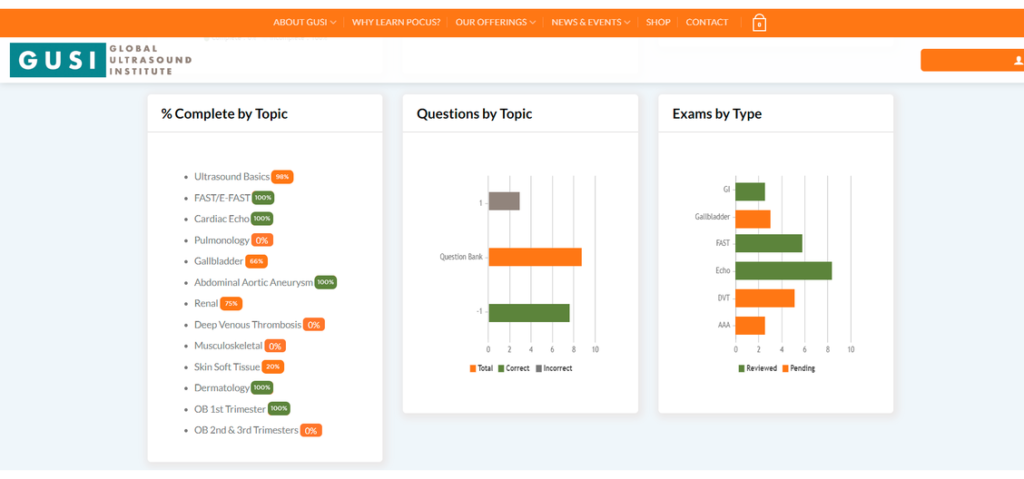
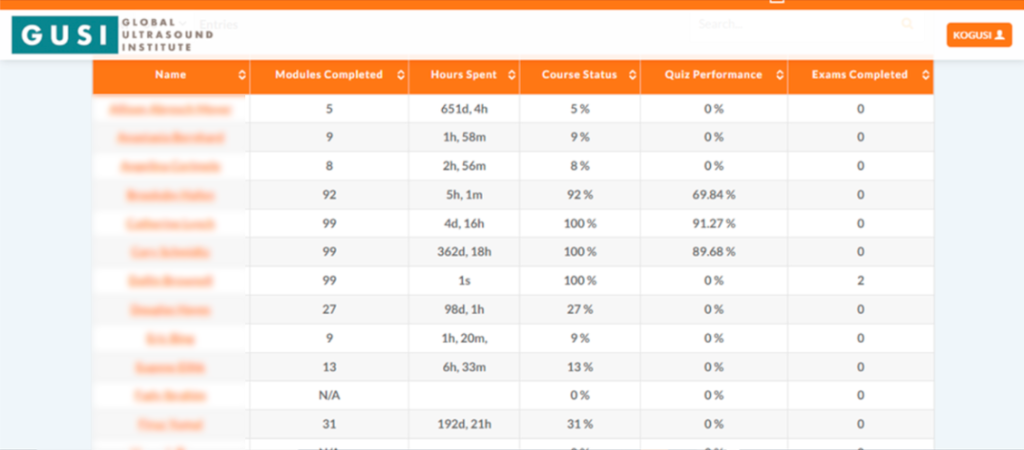
You can build your scan portfolio which you will have lifetime access to and meet the scan requirements established by the AAFP Guidelines and ACEP Guidelines. So no matter where you are in practice, you can take your POCUS portfolio with you.

41 y-o male with a history of hypertension and myopia presents with complete vision loss in his right eye. There is no pain, no tearing, no secretions, or history of trauma. Physical exam shows no light reflex of the right eye. Under direct ophthalmoscope, it is difficult to differentiate any structures, especially with a non dilated eye. You decide to use your ultrasound to evaluate the globe and the posterior structures of the eye.
What is your diagnosis?
Dx: Retinal detachment
Bedside Ultrasound can be used to easily diagnose retinal detachment (RD) , vitreous hemorrhage (VH) , or posterior vitreous detachment (PVD) , especially in patients that present with patients that present with painless vision loss (Lahman et al.)
Bedside ultrasound has a 94.2% sensitivity and 96.3% specificity for retinal detachment, with a positive likelihood ratio of 25.2 and a negative likelihood ratio of 0.06. Moreover, accuracy was not significantly different when it was performed by ED or non-Ed providers. (Gottlieb et al.)
To acquire, a better image remember to use a tegaderm on the patients´ closed eye, use abundant ultrasound gel, and if possible have it cool. This increases the gel’s viscosity, making it easier for the ultrasonographer to apply less pressure and discomfort for the patient. (Soni et al.)
Distinguishing between retinal detachment and posterior vitreous detachment can be challenging, some features that can help you distinguish between the two is that in a RD is directly attached to the optic nerve, it is uniformly thick, more echogenic than a PVD, and less mobile with ocular movements. In contrast, a PVD can cross the optic nerve, it is usually thinner, less echogenic, more mobile with ocular movements and it often presents with hemorrhage. (Baker et al.)
Other Pearls: Remember to always look at the patient’s eye in a transverse and sagittal view and ask the patient to slowly move the eye from one side to the other as this will help you see the whole of the eye and differentiate between a retinal detachment vs. a posterior vitreous.
GUSI POCUS In-Person Courses

Our renowned flagship course, POCUS for Primary Care is coming up April 13-14 in San Francisco! We would love to see you there!
Check out footage from our last POCUS for Primary Care In Person Workshop.
GUSI POCUS Webinars
We host webinars on a wide range of POCUS topics. Access ALL prior webinars here and if you don’t see a webinar on a topic you’d like us to include, let us know and we will happily put it in the queue for future webinars!
Stay tuned for future webinars on POCUS in FQHC’s and An Overview of Equipment Options. Check out our webinar below on How to Implement a Curriculum in your Residency Program
Dr. Paul Bornemann will be joined by Dr. Denis Mahar (Chief of Cardiology, Contra Costa Regional Medical Center), Dr. Floyd Bell (Chair of Radiology, University of South Carolina School of Medicine), Dr. Rob Ferre (POCUS Director for the Indiana University Health System), and Robert Haddad (Sonographer, USC School of Medicine) to discuss how to build partnerships across specialties to support a #POCUS program.
Dr. Paul Bornemann, MD RMSK RPVI, Program Director of the Family Medicine Residency Program, and Director of Primary Care Ultrasound, School of Medicine Columbia, University of South Carolina. He is the lead author for the textbook, Ultrasound for Primary Care. Get your copy here
Coming Soon!
Our website will soon host exciting and educational content around POCUS in the setting of Obstetrics, Tropical Medicine, Ultrasound Guided Nerve Blocks, Ultrasound in Critical Care and POCUS in Resource Limited Settings. Learn more here.
Best wishes and Happy New Year!
Kevin, Mena, and the GUSI Team
Sign up for GUSI’s e-newsletter and updates here.


