News and Information
Spotlight On: Neonatal POCUS

In this article, we are covering the expanding field of neonatal point-of-care ultrasound (POCUS), and paving the way for GUSI’s soon-to-launch neonatal POCUS curriculum!
Despite the extensive adoption of POCUS in adult and pediatric medicine, neonatology’s embrace of this tool in the U.S. has been tentative until recent years. And yet, POCUS is an especially critical tool for management of neonates: this population highly benefits from avoiding radiation, and the immature neonatal bone structure allows for unique ultrasound applications in the brain which are not possible in older children and adults.
Internationally, countries like Australia and New Zealand have pioneered its use more than two decades ago, particularly in cardiac evaluations in Neonatal Intensive Care Units (NICUs). Neonatologist-performed echocardiography (ECHO) in the NICU increased to 90% by 2009 in these countries (Evans et al 2011). In Canada, 78% of neonatal-perinatal medicine programs reported using neonatal POCUS, with 67% reporting POCUS being taught to trainees, but only 22% reporting a formal curriculum according to a 2019 survey (Ben et al 2019). In Italy, 94% of NICUs utilize ECHO with neonatologists performing the majority of the studies for evaluating conditions such as patent ductus arteriosus, pulmonary hypertension, hypotension/shock, cardiac tamponade or for line placement (Corsini et al 2019).
In contrast, a 2011 survey demonstrated that 16% of NICUs utilized POCUS and only 8% had a neonatologist proficient in performing echocardiography (Shepherd 2012). The same survey noted the most common perceived barriers to implementation were:
- Lack of training/maintenance of skills (88%)
- Cost of equipment (53%)
- Medico-legal Concerns (48%)
For NICUs not using POCUS, 75% believed POCUS could be helpful in neonatal care. A more recent study in 2016 reported that 28% of all US neonatologists had used POCUS with 92% reporting lack of training as the major challenge to implementation (Mirza et al 2017).
Recently, international expert consensus for Crashing Neonate Protocols (CNP) have been established (Elsayed et al 2023). A technical report from the American Academy of Pediatrics (AAP) compiled a comprehensive guide for the use of POCUS in the NICU for diagnostic and procedural purposes including cranial, lung, abdominal, and cardiac applications (Stewart et al 2022).
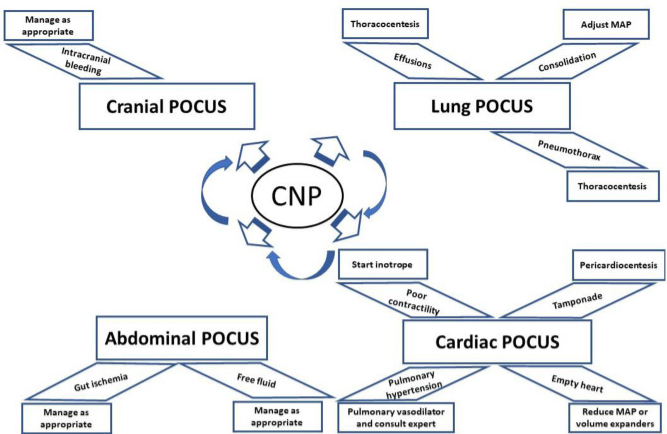
From guiding central catheter placements to assessing lung conditions and even performing critical procedures like thoracentesis, POCUS can be a powerful tool in the NICU setting. It provides a non-invasive view into the smallest patients, yielding immediate insights that can pivot treatment pathways toward better outcomes. In an effort to close the knowledge gap and increase POCUS utilization in the NICU setting, GUSI is pleased to announce the upcoming release of our Neonatal POCUS curriculum this year!
Join us, and be a part of a new chapter in neonatal medicine!
Case #1
![]() A 38-week male infant weighing 4.5 kgs (LGA) was delivered emergently via C-section due to fetal distress. The infant was in respiratory distress initially and required vigorous positive pressure ventilation. The neonate was intubated following resuscitation for surfactant administration and immediately developed respiratory distress, hypotension, and tachycardia. Given the neonate’s resuscitation history and known sequelae of surfactant administration, pneumothorax was suspected. A lung ultrasound was obtained prior to chest radiograph.
A 38-week male infant weighing 4.5 kgs (LGA) was delivered emergently via C-section due to fetal distress. The infant was in respiratory distress initially and required vigorous positive pressure ventilation. The neonate was intubated following resuscitation for surfactant administration and immediately developed respiratory distress, hypotension, and tachycardia. Given the neonate’s resuscitation history and known sequelae of surfactant administration, pneumothorax was suspected. A lung ultrasound was obtained prior to chest radiograph.
The following images were obtained:
A lack of pleural sliding and “barcode sign” on M-mode confirmed the presence of pneumothorax. We again used ultrasound to identify rib spaces, absence of subclavian vasculature, and cardiac structures prior to needle decompression. Needle decompression evacuated 110 mls of air and as this occurred, the cardiac border came into field as the mediastinal shift resolved.
Case #2
![]()
A 28 week infant had an umbilical venous catheter (UVC) and umbilical arterial catheter (UAC) placed soon after delivery to start central total parenteral nutrition (TPN). On the initial X-rays, both lines were lower than traditional landmarks used to confirm appropriate position of umbilical lines. Per emerging unit practice, POCUS was obtained to verify positioning. Research shows that POCUS is superior to chest radiographs.
POCUS revealed that the UVC was in the right atrium. This increases the patient’s risk of a pericardial effusion and/or arrhythmia. The line was retracted under ultrasound guidance. Saline was injected to better visualize the tip.
(cases contributed by Dr. Monti Sharma)
Resources
Evans, N., Gournay, V., Cabanas, F., Kluckow, M., Leone, T., Groves, A., … & Mertens, L. (2011, February). Point-of-care ultrasound in the neonatal intensive care unit: international perspectives. In Seminars in Fetal and Neonatal Medicine (Vol. 16, No. 1, pp. 61-68). WB Saunders.
Ben Fadel, N., Pulgar, L., & Khurshid, F. (2019). Point of care ultrasound (POCUS) in Canadian neonatal intensive care units (NICUs): where are we?. Journal of Ultrasound, 22, 201-206.
Corsini, I., Ficial, B., Fiocchi, S., Schena, F., Capolupo, I., Cerbo, R. M., … & Study Group of Neonatal Cardiology of the Italian Society of Neonatology. (2019). Neonatologist performed echocardiography (NPE) in Italian neonatal intensive care units: a national survey. Italian Journal of Pediatrics, 45, 1-7.
Shepherd, J., Mukthapuram, S., & Kim, J. H. (2022, October). Neonatal POCUS: Embracing our modern day “stethoscope”. In Seminars in Fetal and Neonatal Medicine (Vol. 27, No. 5, p. 101394). WB Saunders.
Mirza, H. S., Logsdon, G., Pulickal, A., Stephens, M., & Wadhawan, R. (2017). A national survey of neonatologists: barriers and prerequisites to introduce point-of-care ultrasound in neonatal ICUs. Ultrasound Quarterly, 33(4), 265-271.
Elsayed Y, Wahab MGA, Mohamed A, Fadel NB, Bhombal S, Yousef N, Fraga MV, Afifi J, Suryawanshi P, Hyderi A, Katheria A, Kluckow M, De Luca D, Singh Y. Point-of-care ultrasound (POCUS) protocol for systematic assessment of the crashing neonate-expert consensus statement of the international crashing neonate working group. Eur J Pediatr. 2023 Jan;182(1):53-66. doi: 10.1007/s00431-022-04636-z. Epub 2022 Oct 14. PMID: 36239816; PMCID: PMC9829616.
Dan L. Stewart, Yasser Elsayed, María V. Fraga, Brian D. Coley, Aparna Annam, Sarah Sarvis Milla, COMMITTEE ON FETUS AND NEWBORN AND SECTION ON RADIOLOGY; Use of Point-of-Care Ultrasonography in the NICU for Diagnostic and Procedural Purposes. Pediatrics December 2022; 150 (6): e2022060052. 10.1542/peds.2022-060052

I hope I can join this course as soon as possible.